- Research article
- Open access
- Published:
Minimally invasive surgeries for spontaneous hypertensive intracerebral hemorrhage (MISICH): a multicenter randomized controlled trial
BMC Medicine volume 22, Article number: 244 (2024)
Abstract
Background
Intracerebral hemorrhage (ICH) is a common stroke type with high morbidity and mortality. There are mainly three surgical methods for treating ICH. Unfortunately, thus far, no specific surgical method has been proven to be the most effective. We carried out this study to investigate whether minimally invasive surgeries with endoscopic surgery or stereotactic aspiration (frameless navigated aspiration) will improve functional outcomes in patients with supratentorial ICH compared with small-bone flap craniotomy.
Methods
In this parallel-group multicenter randomized controlled trial conducted at 16 centers, patients with supratentorial hypertensive ICH were randomized to receive endoscopic surgery, stereotactic aspiration, or craniotomy at a 1:1:1 ratio from July 2016 to June 2022. The follow-up duration was 6 months. Patients were randomized to receive endoscopic evacuation, stereotactic aspiration, or small-bone flap craniotomy. The primary outcome was favorable functional outcome, defined as the proportion of patients who achieved a modified Rankin scale (mRS) score of 0–2 at the 6-month follow-up.
Results
A total of 733 patients were randomly allocated to three groups: 243 to the endoscopy group, 247 to the aspiration group, and 243 to the craniotomy group. Finally, 721 patients (239 in the endoscopy group, 246 in the aspiration group, and 236 in the craniotomy group) received treatment and were included in the intention-to-treat analysis. Primary efficacy analysis revealed that 73 of 219 (33.3%) in the endoscopy group, 72 of 220 (32.7%) in the aspiration group, and 47 of 212 (22.2%) in the craniotomy group achieved favorable functional outcome at the 6-month follow-up (P = .017). We got similar results in subgroup analysis of deep hemorrhages, while in lobar hemorrhages the prognostic outcome was similar among three groups. Old age, deep hematoma location, large hematoma volume, low preoperative GCS score, craniotomy, and intracranial infection were associated with greater odds of unfavorable outcomes. The mean hospitalization expenses were ¥92,420 in the endoscopy group, ¥77,351 in the aspiration group, and ¥100,947 in the craniotomy group (P = .000).
Conclusions
Compared with small bone flap craniotomy, endoscopic surgery and stereotactic aspiration improved the long-term outcome of hypertensive ICH, especially deep hemorrhages.
Trial Registration
ClinicalTrials.gov Identifier: NCT02811614.
Background
Stroke is a leading cause of mortality and disability worldwide, and the economic costs of treatment and poststroke care are substantial [1, 2]. Although the prevalence of intracerebral hemorrhage (ICH) is only approximately one-quarter that of ischemic stroke, the cause-specific death and years of life lost due to ICH exceed those of ischemic stroke [3,4,5]. Death from ICH is estimated to occur in 30% to 40% of cases, and most patients who survive ICH have disabilities and are at risk for recurrent stroke [6]. The incidence of ICH increases sharply with age and is therefore expected to remain substantial as the population ages, even with improvements in blood pressure control [7].
Theoretically, surgery has the advantages of reducing hematoma volume and relieving perihematomal edema compared with conservative treatment [8, 9]. However, findings from randomized controlled trials (RCTs) have shown that for most patients with supratentorial ICH, the effectiveness of craniotomy for hemorrhage evacuation to improve functional outcome or mortality is uncertain [10, 11]. An important factor that affects the effectiveness of craniotomy is the damage to normal brain tissue caused by surgery. Compared with conventional craniotomy, minimally invasive surgery for ICH can minimize the disruption of healthy brain tissue. Two main types of minimally invasive surgery have been attempted for hematoma removal: endoscopic surgery and stereotactic aspiration [12, 13]. To date, except for some retrospective studies or meta-analyses [14,15,16], no large-scale RCT comparing these three surgical interventions have been reported. Therefore, we designed the minimally invasive surgeries for spontaneous hypertensive intracerebral hemorrhage (MISICH) trial to investigate whether endoscopic surgery and/or stereotactic aspiration (frameless navigated aspiration) would improve functional outcomes in patients with supratentorial ICH compared with small-bone flap craniotomy.
Methods
Study design
MISICH is a multicenter, randomized controlled, open-label, sequentially designed nonprofit study (ClinicalTrials.gov ID: NCT02811614) involving 16 neurosurgical centers across China. The study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines and was in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics committees of the Chinese PLA General Hospital (S2016-074–01). Details about the trial design, conduct, and oversight can be found in the trial protocol in Additional file 1 and published elsewhere [17].
Participants
The inclusion criteria included supratentorial hypertensive ICH patients who were 18 to 80 years of age, had a hemorrhage volume ≥ 25 mL, were admitted to the hospital within 24 h of ictus, had a Glasgow Coma Scale (GCS) score ≥ 5, and had a modified Rankin scale (mRS) score of 0 or 1 before hemorrhage. The exclusion criteria included concurrent head injury or cerebral tumor, multiple bleeding events, brain herniation at admission, hemorrhage due to aneurysm or arteriovenous malformation, and pregnancy. Detailed inclusion and exclusion criteria were presented in Additional file 1. All the chief surgeons who participated in this study had been involved in neurosurgery for more than 15 years and participated in training programs held by the Chinese PLA General Hospital. All the chief surgeons were proficient in all three surgical methods before recruiting patients.
Randomization
Patients were randomly allocated to endoscopy group, aspiration group, or craniotomy group at a 1:1:1 ratio using a randomization system based on computer-generated number sequences after providing written informed consent. Complete randomization was used to minimize selection bias, and neither the neurosurgeons nor the patients were familiarized with the grouping beforehand. Randomization was completed within 24 h of hemorrhage, and patients were operated on within 12 h after randomization. The independent study statistician was blinded to the grouping information. Blinding of treating neurosurgeons and investigators was infeasible due to the nature of the surgery.
Procedures
In contrast to the method used in previous studies, we used the open-source software 3D Slier (http://www.slicer.org/) to reconstruct and digitally measure the volume of hematoma since the traditional ABC/2 method usually overestimates hematoma volume, especially for irregular hematomas [18]. The process of hematoma 3D reconstruction was presented in Appendix 1 in Additional file 2. Accurate measurement of hematoma volume by computer could reduce estimation error and improve the comparability of data between participating centers. CT angiography (CTA) was performed when the underlying vascular pathology was suspected to be a source of bleeding. The indications for CTA included lobar hemorrhage in patients younger than 70 years, deep hemorrhage in patients younger than 45 years, and subarachnoid hemorrhage.
In the endoscopic surgery group, a bone flap approximately 2 cm in diameter was made according to the position of the hemorrhage. Surgical approaches included the middle frontal gyrus approach for basal ganglia hemorrhage, the parietooccipital approach for thalamic hemorrhage, and the subcortical approach for superficial lobar hemorrhage. Using a self-developed neuro-endoport (Chinese invention patent number: 201210066281.1), a transparent working channel was made to evacuate the hematoma under endoscopic surveillance [19]. Thrombolytic agents were not used after surgery. In the stereotactic aspiration group, the target point was set near the posterior edge of the hematoma on CT, which was the location at which the largest expansion of the hematoma occurred. Available commercial frameless neuro-navigation or free mobile-device-based navigation, rather than stereotactic head frame, was used to improve the accuracy of catheter puncture [20]. Initial hematoma aspiration was performed intraoperatively immediately after catheter insertion. After confirmation of the catheter by postoperative CT, urokinase (30,000 units every 12 h) was injected through the catheter to dissolve residual hematoma for 3–5 days [21]. The catheter was removed when there was no additional blood drained or when the catheter had been placed for 5 days. In the small-boneflap craniotomy group, the chief surgeon chose a suitable surgical approach based on the hemorrhage location and made a minimal boneflap to evacuate the hematoma as much as possible under microscope. Decompressive craniectomy was performed only when the brain tissue swelled significantly after hematoma evacuation. All patients were then transferred to the neurosurgical intensive care unit (NICU) until they were evaluated as stable enough for the general ward. We followed the guidelines for the management of spontaneous ICH from the American Heart Association and American Stroke Association, which enabled a standard schedule for monitoring patients’ blood pressure, airways, sedation, and pharmacological treatment [22].
Outcomes
The primary outcome was the proportion of patients who achieved a favorable outcome, defined as a mRS score of 0–2 at 6 months after hemorrhage. Patients were adjusted for group differences in the main baseline covariates, such as sex ratio, age, preoperative GCS score, time from onset to surgery, and hematoma volume. Secondary outcomes included quality of life measured with the Barthel Index at the 6-month follow-up, mortality rate at one month, days of NICU stay, hospitalization time, intracranial infection rate, hospitalization expenses, hematoma clearance rate and operation time. The stroke-related pneumonia rate was also recorded as a secondary outcome. Patients were followed-up by investigators blinded to the treatment allocation through online video interviews and questionnaires 1 month and 6 months after treatment. A special case report form (see Appendix 2 in Additional file 2) was designed for data collection and outcome assessment. Adverse events were reported by the investigators throughout the study and were assessed by an independent supervisor (JSZ). An independent data safety and monitoring committee was appointed by the study sponsor.
Statistical analysis
Our previous retrospective study indicated that an estimated 38% of patients in the endoscopy group would have an mRS score of 0–2, but only 17% of craniotomy patients would have the same outcome [19]. We estimated that 720 patients (240 patients in each treatment group) would provide 90% power and a type I error probability of 0.05 to detect an effect size of 12%, with a 10% dropout rate taken into consideration. Statistical analysis was performed on an “intention-to-treat” basis by treatment allocation. The primary outcome analysis was a simple categorical frequency comparison using the chi-square test for prognosis-based favorable or unfavorable outcomes based on the mRS at 6-month follow-up. The secondary outcome analysis consisted of one-way analysis of variance (ANOVA) for continuous variables and logistic regression analysis for age, gender, preoperative GCS score, hematoma location, hematoma volume, surgical method, and intracranial infection. A two-sided P < 0.05 was considered to indicate statistical significance.
Results
Clinical characteristics
Between July 1, 2016, and June 30, 2022, 1226 ICH patients from 16 hospitals across China were screened for eligibility; 733 patients were randomly allocated to the three study groups. Among the 493 patients who were excluded from the trial, 318 (64.5%) did not meet the inclusion criteria, and 175 (35.5%) refused consent. Further 12 patients were excluded due to ineligible hematoma volume or consent withdrawal before treatment and were not included in the analysis. Finally, 721 patients (239 in the endoscopy group, 246 in the aspiration group, and 236 in the craniotomy group) received treatment and were included in the intention-to-treat analysis (Fig. 1). The demographic and baseline characteristics of patients were summarized in Table 1. The results showed that 497 (68.8%) of 721 patients were men and 225 (31.2%) were women (mean age 56.7 years, SD 11.3); 395 (54.8%) were left-sided hemorrhage and 326 (45.2%) were right-sided hemorrhage. For hemorrhage location, 515 (71.4%) were located mainly in the basal ganglia, 144 (20.0%) located in the lobar region, and 62 (8.6%) located in the thalamus. Forty-eight (20.1%) patients in the endoscopy group, 53 (21.5%) patients in the aspiration group, and 42 (17.8%) patients in the craniotomy group involved intraventricular hemorrhage (P = 0.598). The mean Graeb score of these patients were 2.5 (SD 0.8) in the endoscopy group, 2.7 (SD 1.0) in the aspiration group, and 2.6 (SD 0.9) in the craniotomy group (P = 0.264). On admission, the mean hematoma volume was 49.2 mL (SD 17.7, range 25.0–112.3), and the median GCS score was 9 (IQR 7–11). Medical conditions, past medical history, and the proportion of patients taking anticoagulants were similar among three groups. The preoperative characteristics of patients were balanced and comparable among three groups.
The mean hematoma clearance rate was 88.3% (SD 20.8) in the endoscopy group, 60.3% (SD 25.6) in the aspiration group, and 86.5% (SD 17.9) in the craniotomy group (P = 0.000). The time required for surgery was 1.0 h in the aspiration group, 2.0 h in the endoscopy group, and 3.5 h in the craniotomy group (P = 0.000). In terms of intraoperative blood loss, endoscopy (88 mL) and aspiration (38 mL) was less than that of craniotomy (268 mL) (P = 0.000). The percentage of patients receiving intraoperative blood transfusion was 8.4% (20/239) in the endoscopy group, 2.8% (7/246) in the aspiration group, and 24.6% (58/236) in the craniotomy group, with statistical significance (P = 0.000). Nearly one-third of patients in the craniotomy group (31.9%, 75/236) developed stroke-related pneumonia, which was higher than that in the endoscopy group (22.6%, 54/239) and the aspiration group (18.3%, 45/246), the difference was statistically significant (P = 0.002). The incidence of intracranial infection was 4.6% (11/239) in the endoscopy group, 6.9% (17/246) in the aspiration group, and 5.9% (14/236) in the craniotomy group, with no statistically significant difference (P = 0.553). The median time in NICU was 5 days in the endoscopy group, 4 days in the aspiration group, and 6 days in the craniotomy group (P = 0.042), though the median hospitalization time were similar among three groups (22 vs 23 vs 23, P = 0.083). The mean hospitalization expenses were ¥92,420 in endoscopy group, ¥77,351 in aspiration group, and ¥100,947 in craniotomy group (P = 0.000). Stereotactic aspiration was the most economical surgical method. The general clinical results were summarized in Table 2.
Functional outcome
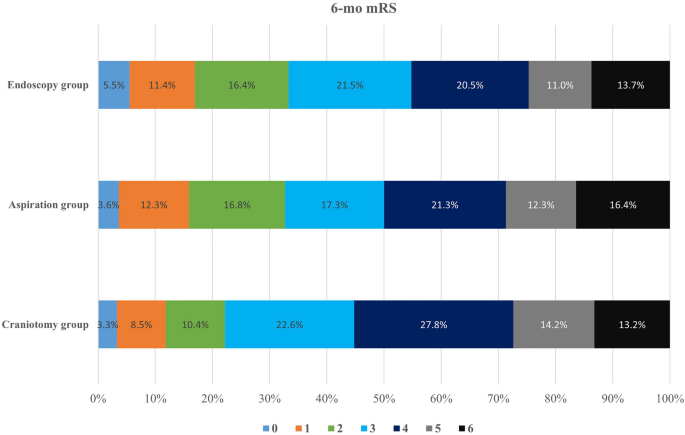
Ten patients in the endoscopy group, 13 patients in the aspiration group, and 14 patients in the craniotomy group crossover to other treatment groups. The reasons for cross-over contained refusal by relatives (18), neurological deterioration (8), relative contradiction for craniotomy or endoscopic surgery due to other major clinical event (6), and reason not recorded (5). The statistical analysis was based on initial grouping. At 6 months after ictus, 70 patients were lost to follow-up. Of the 651 patients with available mRS scores and BI scores at 6-month follow-up, 73 (33.3%) of 219 patients in the endoscopy group, 72 (32.7%) of 220 patients in the aspiration group, and 47 (22.2%) of 212 patients in the craniotomy group achieved a mRS score of 0–2. The long-term prognosis outcome was presented in Table 3. The proportion of patients with favorable outcome in the endoscopy group and the aspiration group was greater than that in the craniotomy group (Fig. 2, P = 0.017). Compared with small-boneflap craniotomy, the prognostic advantage of endoscopic surgery was 11.1% and that of frameless navigated aspiration was 10.5%. The 6-month mortality was 13.7% (30/219) in the endoscopy group, 15.0% (33/220) in the aspiration group, and 16.5% (35/212) in the craniotomy group. The difference was insignificant (P = 0.717). The median Barthel Index of alive patients at 6-month follow-up was 75 (IQR 45–95) in the endoscopy group, 75 (IQR 55–95) in the aspiration group, and 70 (IQR 40–90) in the craniotomy group. Patients in the endoscopy group and the aspiration group got better quality of lives than those in the craniotomy group (P = 0.019).
Age, gender, preoperative GCS score, hematoma location, hematoma volume, surgical method, and intracranial infection were included in the non-conditional logistic regression analysis to identify any variable that correlated with patients’ functional outcome. Young age, better preoperative GCS score, small hematoma volume, lobar hematoma location, endoscopic surgery or stereotactic aspiration, and no intracranial infection were associated with higher odds of favorable outcome (6-month mRS 0–2). The odds ratios for age, preoperative GCS score, hematoma volume, endoscopic surgery, stereotactic aspiration, and intracranial infection were 1.046 (P = 0.000), 0.848 (P = 0.00), 6.159 (P = 0.000), 1.034 (P = 0.000), 0.383 (P = 0.000), 0.453 (P = 0.003), and 6.518 (P = 0.004), respectively (Table S1 in Additional file 2). Further analysis showed that for patients with supratentorial deep hemorrhages (basal ganglia hemorrhages and thalamus hemorrhages), the probability of achieving a favorable outcome was 30.3% (54/178) for endoscopic surgery, 28.4% (50/176) for stereotactic aspiration, and 14.8% (25/169) for craniotomy. The results had a significant statistical difference (P = 0.001). For patients with supratentorial lobar hemorrhages, the probability of achieving a favorable outcome was 46.3% (19/41) for endoscopic surgery, 50.0% (22/44) for stereotactic aspiration, and 51.2% (22/43) for craniotomy. The prognosis of craniotomy surgery was slightly better, but the difference was not statistically significant (P = 0.900). The probability of achieving a favorable outcome was similar between left-sided ICH (30.0%, 88/293) and right-sided ICH (29.6%, 106/358) (P = 0.542). Among the 125 followed-up patients with a GCS score of greater than or equal to 13 before surgery, 54.8% (23/42) in the endoscopic surgery, 53.5% (23/43) in the stereotactic aspiration, and 42.5% (17/40) in the craniotomy achieved a favorable outcome. The difference did not reach statistical significance (P = 0.477).
Specified safety event (such as severe rebleeding or sudden brain herniation) rates did not reach the predetermined review threshold throughout the trial. In the endoscopy group, 9 of 239 (3.8%) patients experienced rebleeding after surgery, and 6 patients underwent reoperation. Furthermore, one patient received external ventricular drainage because of hydrocephalus after hemorrhage, one patient underwent third ventriculostomy and fistulation of the entrapped temporal horn, and one patient suffered from bleeding at tracheotomy. In the aspiration group, 15 of 246 (6.1%) patients experienced rebleeding after surgery, 4 patients underwent a second-time stereotactic aspiration, and 2 patients underwent craniotomy. Two patients received external ventricular drainage because of hydrocephalus after hemorrhage. In the craniotomy group, 12 of 236 (5.1%) patients experienced rebleeding after surgery, and 7 patients underwent craniotomy again. Three patients received external ventricular drainage because of hydrocephalus. Decompressive craniotomy was performed in only 8 patients (3.4%) in the craniotomy group. The percentage of patients suffering from rebleeding did not reach statistical significance. At the 1-month follow-up, the mortality rates were similar among the three groups (17/239, 7.1% vs 20/246, 8.1% vs 19/236, 8.1%, P = 0.898). Until 6-month follow-up, 11 patients in the endoscopy group, 24 patients in the aspiration group, and 20 patients in the craniotomy group develop hydrocephalus that required shunt surgery. The difference was insignificant (P = 0.052).
Discussion
As the deadliest form of acute stroke, ICH has been a great public health threat with persistently high mortality in recent decades [4, 7, 23]. Novel treatments and improved application of established approaches are needed for ICH [22]. The usefulness of craniotomy for most patients with spontaneous supratentorial ICH of moderate severity remains uncertain [10, 11, 24,25,26,27]. For large supratentorial ICH accompanied with clinical deterioration and significant midline shift, decompressive craniectomy with or without hematoma evacuation is considered a lifesaving procedure [24, 28]. A variety of possible reasons have been proposed for why craniotomy fails to improve ICH outcomes, including operation beyond the optimal treatment time, insufficient sample size, incomplete hematoma removal, and relatively high cross rate between groups. The damage to normal brain tissue caused by surgery and its impact on the postoperative recovery of patients have not been thoroughly studied.
There is still a long way to go in the clinical research of ICH. The STICH study compared early surgery with initial conservative treatment for patients with ICH and the results showed that early surgery had no benefit compared with initial conservative treatment. The STICH II study demonstrated that early surgery might have a small but clinically relevant survival advantage for patients with superficial ICH. The MISTIE III study found that for moderate to large ICH, minimally invasive catheter evacuation followed by thrombolysis did not improve the proportion of patients who achieved a good response 365 days after ICH compared with standard medical treatment. STICH and STICH II used the 8 point extended Glasgow Outcome Scale (GOS) and MISTIE III used the modified Rankin Scale (mRS). The proportion of patients with favorable outcome was 26% and 24% in STICH, 41% and 38% in STICH II, and 45% and 41% in MISTIE III [10, 11, 13]. Recently, minimally invasive surgeries have the appeal of relieving hematoma volume, reducing perihematomal edema, and minimizing disruption of healthy brain tissue. Minimally invasive surgeries were reported to be helpful for reducing mortality and improving functional outcomes compared with conventional craniotomy or standard medical treatment [12,13,14,15,16] [29,30,31,32]. Studies comparing minimally invasive surgery with craniotomy were all small sample RCTs, retrospective data or meta-analysis. In this multicenter large-scale RCT, endoscopic surgery and stereotactic aspiration improved functional outcomes compared with craniotomy in patients with supratentorial ICH. At 6-month follow-up, 33.3% patients in the endoscopy group and 32.7% patients in the aspiration group achieved a favorable outcome (mRS score 0–2), which was significantly greater than that (22.2%) in the craniotomy group. Patients who underwent minimally invasive surgeries also got better quality of lives. The prognosis advantage of endoscopic surgery and stereotactic aspiration over craniotomy was mainly reflected in patients with deep hemorrhages. For patients with superficial lobar hemorrhages, there was no statistically significant difference in the prognostic outcomes among the three surgical methods. The proportion of patients with lobar hemorrhage in our study was relatively small, and the results warranted further investigation.
There was no significant difference in mortality at 6 months after hemorrhage. Previous studies have shown that for patients with supratentorial ICH and intraventricular hemorrhage, endoscopic surgery or stereotactic aspiration with or without thrombolytic use reduces mortality compared with craniotomy [12, 13, 33, 34]. The reasons for the similar 6-month mortality in three groups might be that the overall mortality of the enrolled patients was relatively low, some patients were lost to follow-up or crossed over, and our 6-month follow-up did not record the specific cause of death. Furthermore, our results provide important health economic evidence that stereotactic aspiration is the most economical surgical method. Our study provides important new evidence for minimally invasive treatment of spontaneous hypertensive ICH. Apart from deep hemorrhage location, occurrence of intraventricular hemorrhage (IVH) was also was an important predictor of poor outcome. Post-hemorrhagic hydrocephalus develops in 30%-50% of patients with IVH [35]. Endoscopic surgery was reported to not only improve the prognosis but also reduce shunt dependence after IVH [36]. Patients with pure IVH or IVH volume exceeding 50% of the total hematoma volume were not included in our study, therefore, the proportion of IVH in our series was low and the difference did not reach statistical significance.
A follow-up rate of 90.3% was achieved, and the crossover rate was controlled to a relatively low level. The MISICH trial used the intention-to-treat principle; that is, the analysis of outcomes was based on the patients’ initial randomization results rather than the final treatment that the patient received to avoid the influence of human factors that may influence the results. All three surgical methods were safe regarding serious rebleeding and intracranial infection, and no obvious procedural risk was reported in all groups. The potential impact of the timing of surgery for ICH on outcome remains controversial, and the best therapeutic time window is unknown [32, 37]. STICH I and STICH II did not identify an early time effect [10, 11]. In MISICH, surgery was performed at 6-48 h since hematoma expansion, an indication of unfavorable outcome, occurred in nearly one third patients and mostly occurred within 6 h after haemorrhage [38, 39]. No surgery was performed within 6 h in our study. Further research evaluating the best surgery timing was warranted. The relationship between hematoma clearance rate and patient prognosis remains unclear. The hematoma clearance rate of stereotactic aspiration was lower than that of craniotomy, but the recovery of neurological function was better, indicating that within a certain range, increasing hematoma clearance rate could improve prognosis; however, when the hematoma is cleared to a certain extent, further removal of hematoma could not provide additional benefit. The cutoff clearance rate is still unknown and it is generally recommended to remove the hematoma until the residual hematoma volume is less than 15 ml [11, 13, 22, 24]. We conducted subgroup analysis based on whether the residual hematoma volume was greater than 15 ml. The results showed that 31.9% (151/475) of patients with residual hematoma less than 15 ml achieved a favorable outcome (mRS 0–2) versus 23.0% (41/178) of patients with residual hematoma more than or equal to 15 ml achieved a favorable outcome (P = 0.017).
This study has several limitations. First, insufficient power might be an issue due to the moderate size of the intention-to-treat analysis, while dichotomous variables (favorable or unfavorable) usually require a large sample size. Second, the inclusion criteria might exclude some patients with unfavorable prognosis and whether patients with GCS scores of 5 suitable for enrollment left room for discussion. Third, the number of patients recruited from participating centers differed, potentially resulting in regional biases, which might be a confounding factor.
Conclusions
This prospective multicenter RCT demonstrated that, compared with small-bone flap craniotomy, endoscopic surgery and frameless navigated aspiration significantly improved the functional outcomes and quality of life of patients with moderate to large supratentorial hypertensive ICH, especially deep hemorrhages. Frameless navigated aspiration and endoscopic surgery were also more cost-effective compared with small-bone flap craniotomy. More powered clinical data are warranted to compare endoscopic surgery with stereotactic aspiration.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ANOVA:
-
One-way analysis of variance
- GCS:
-
Glasgow Coma Scale
- ICH:
-
Intracerebral hemorrhage
- IQR:
-
Interquartile range
- IVH:
-
Intraventricular hemorrhage
- MISICH:
-
Minimally invasive surgeries for spontaneous hypertensive intracerebral hemorrhage
- mRS:
-
Modified Rankin Scale
- NICU:
-
Neurosurgical intensive care unit
- SD:
-
Standard deviation
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Rajsic S, Gothe H, Borba HH, et al. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ. 2019;20:107–34.
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820.
GBD 2017 US Neurological Disorders Collaborators, Feigin VL, Vos T, et al. Burden of Neurological Disorders Across the US From 1990-2017: A Global Burden of Disease Study. JAMA Neurol. 2021;78:165–76.
Guan T, Ma J, Li M, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology. 2017;89:53–61.
Sheth KN. Spontaneous Intracerebral Hemorrhage. N Engl J Med. 2022;387:1589–96.
Jolink WM, Klijn CJ, Brouwers PJ, Kappelle LJ, Vaartjes I. Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology. 2015;85:1318–24.
Vespa PM, Martin N, Zuccarello M, Awad I, Hanley DF. Surgical trials in intracerebral hemorrhage. Stroke. 2013;44:S79–82.
Xi G, Keep RF, Hoff JT. Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol. 2006;5:53–63.
Mendelow AD, Gregson BA, Fernandes HM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005;365:387–97.
Mendelow AD, Gregson BA, Rowan EN, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382:397–408.
Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989;70:530–5.
Hanley DF, Thompson RE, Rosenblum M, et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. 2019;393:1021–32.
Ding W, Xiang Y, Liao J, Wang X. Minimally invasive puncture versus conventional craniotomy for spontaneous supratentorial hemorrhage: A meta-analysis. Neurochirurgie. 2021;67:375–82.
Sondag L, Schreuder FHBM, Boogaarts HD, et al. Neurosurgical Intervention for Supratentorial Intracerebral Hemorrhage. Ann Neurol. 2020;88:239–50.
Sun S, Li Y, Zhang H, et al. Neuroendoscopic Surgery versus Craniotomy for Supratentorial Hypertensive Intracerebral Hemorrhage: A Systematic Review and Meta-Analysis. World Neurosurg. 2020;134:477–88.
Xu X, Zheng Y, Chen X, Li F, Zhang H, Ge X. Comparison of endoscopic evacuation, stereotactic aspiration and craniotomy for the treatment of supratentorial hypertensive intracerebral haemorrhage: study protocol for a randomised controlled trial. Trials. 2017;18:296.
Xu X, Chen X, Zhang J, et al. Comparison of the Tada formula with software slicer: precise and low-cost method for volume assessment of intracerebral hematoma. Stroke. 2014;45:3433–5.
Xu X, Chen X, Li F, et al. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: a comparison with craniotomy. J Neurosurg. 2018;128:553–9.
Li F, Gan Z, Xu X, et al. Smartphone navigated endoscopic port surgery of hypertensive basal ganglia hemorrhage. J Clin Neurosci. 2022;101:193–7.
Yu Z, Tao C, Xiao A, et al. Chinese multidisciplinary guideline for management of hypertensive intracerebral hemorrhage. Chin Med J (Engl). 2022;135:2269–71.
Hemphill JC 3rd, Greenberg SM, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54:171–9.
Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2022;53:e282–361.
Guo G, Pan C, Guo W, et al. Efficacy and safety of four interventions for spontaneous supratentorial intracerebral hemorrhage: a network meta-analysis. J Neurointerv Surg. 2020;12:598–604.
Li M, Mu F, Su D, Han Q, Guo Z, Chen T. Different surgical interventions for patients with spontaneous supratentorial intracranial hemorrhage: A network meta-analysis. Clin Neurol Neurosurg. 2020;188:105617.
Moussa WM, Khedr W. ompressive craniectomy and expansive duraplasty with evacuation of hypertensive intracerebral hematoma, a randomized controlled trial. Neurosurg Rev. 2017;40:115–27.
Fung C, Murek M, Z’Graggen WJ, et al. ompressive hemicraniectomy in patients with supratentorial intracerebral hemorrhage. Stroke. 2012;43:3207–11.
Gildersleeve KL, Hirzallah MI, Esquenazi Y, et al. Hemicraniectomy for Supratentorial Primary Intracerebral Hemorrhage: A Retrospective, Propensity Score Matched Study. J Stroke Cerebrovasc Dis. 2019;28: 104361.
Hegde A, Prasad GL, Menon G. ompressive Craniectomy in Spontaneous Intracerebral Hemorrhage: A Comparison with Standard Craniotomy Using Propensity-Matched Analysis. World Neurosurg. 2020;144:e622–30.
Cho DY, Chen CC, Chang CS, Lee WY, Tso M. Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol. 2006;65:547–56.
Wang WZ, Jiang B, Liu HM, et al. Minimally invasive craniopuncture therapy vs. conservative treatment for spontaneous intracerebral hemorrhage: results from a randomized clinical trial in China. Int J Stroke. 2009;4:11–6.
Vespa P, Hanley D, Betz J, et al. ICES (Intraoperative Stereotactic Computed Tomography-Guided Endoscopic Surgery) for brain hemorrhage: a multicenter randomized controlled trial. Stroke. 2016;47:2749–55.
Zhou H, Zhang Y, Liu L, et al. A prospective controlled study: minimally invasive stereotactic puncture therapy versus conventional craniotomy in the treatment of acute intracerebral hemorrhage. BMC Neurol. 2011;11:76.
Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD, STICH Investigators. Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl. 2006;96:65–68.
Mei L, Fengqun M, Qian H, Dongpo S, Zhenzhong G, Tong C. Exploration of Efficacy and Safety of Interventions for Intraventricular Hemorrhage: A Network Meta-Analysis. World Neurosurg. 2020;136:382–9.
Ge C, Zhao W, Guo H, et al. Comparison of the clinical efficacy of craniotomy and craniopuncture therapy for the early stage of moderate volume spontaneous intracerebral hemorrhage in basal ganglia: Using the CTA spot sign as an entry criterion. Clin Neurol Neurosurg. 2018;169:41–8.
Polster SP, Carrión-Penagos J, Lyne SB, et al. Intracerebral Haemorrhage Volume Reduction and Timing of Intervention Versus Functional Benefit and Survival in the MISTIE III and STICH Trials. Neurosurgery. 2021;88:961–70.
Pantazis G, Tsitsopoulos P, Mihas C, Katsiva V, Stavrianos V, Zymaris S. Early surgical treatment vs conservative management for spontaneous supratentorial intracerebral hematomas: A prospective randomized study. Surg Neurol. 2006;66:492–502.
Acknowledgements
We thank Xin Ge (Wuxi Nineth Hospital), Wei Wang (Yichang Central People’s Hospital), Xu Zhang (Liaoning Thrombus Hospital), Yilong Peng (Jiangmen Central Hospital), Famu Lin (People’s Hospital of Sanshui District), Huan Lan (Minzu Hospital of Guangxi Medical University), Rui Huang (The Second Hospital of Jilin University), Mo Chen (Jilin Province People’s Hospital), Xiaodong Li (Siping Central People’s Hospital), Yanlong Yang (Tangdu Hospital of Air Force Military Medical University), Ning Jiang (The Third Affiliated Hospital of Inner Mongolia Medical University), and Hu Qin (The First Affiliated Hospital of Xinjiang Medical University) for their significant contributions to patient enrollment and data gathering.
Funding
This study was supported by the National Natural Sciences Foundation of China (No. 82272134 & 81901393) and the National Key R&D Plan of China (No. 2018YFC1312602).
Author information
Authors and Affiliations
Consortia
Contributions
XHX: study design, data collection, analysis, and interpretation, and drafting of the article. HPZ: patient enrollment, data collection. JSZ: data monitoring. ML: patient enrollment, data collection. QW: data collection and analysis. YNZ: data collection. ZCG: designing the case report form, data collection and analysis. BNX: research guidance. XLC: study design, data analysis and interpretation, critical revision of the article. All the authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committees of the Chinese PLA General Hospital (S2016-074–01). Written informed consent was obtained from all participants or their legal representatives.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12916_2024_3468_MOESM2_ESM.docx
Additional file 2: Appendix 1. Digital Hematoma Volume Measurement with 3D Slicer. Appendix 2. MISICH Case Report Form. Table S1. Logistic regression for unfavorable outcome.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, X., Zhang, H., Zhang, J. et al. Minimally invasive surgeries for spontaneous hypertensive intracerebral hemorrhage (MISICH): a multicenter randomized controlled trial. BMC Med 22, 244 (2024). https://doi.org/10.1186/s12916-024-03468-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03468-y