- Research
- Open access
- Published:
Association between social determinants of health and survival among the US cancer survivors population
BMC Medicine volume 22, Article number: 343 (2024)
Abstract
Background
Racial and ethnic disparities in mortality persist among US cancer survivors, with social determinants of health (SDoH) may have a significant impact on these disparities.
Methods
A population-based cohort study of a nationally representative sample of adult cancer survivors, who participated in the US National Health and Nutrition Examination Survey from 1999 to 2018 was included. Sociodemographic characteristics and SDoH were self-reported using standardized questionnaires in each survey cycle. The SDoH was examined by race and estimated for associations with primary outcomes, which included all-cause and cancer-specific mortality. Multiple mediation analysis was performed to assess the contribution of each unfavorable SDoH to racial disparities to all-cause and cancer-specific mortality.
Results
Among 5163 cancer survivors (2724 [57.7%] females and 3580 [69.3%] non-Hispanic White individuals), only 881 (24.9%) did not report an unfavorable SDoH. During the follow-up period of up to 249 months (median 81 months), 1964 deaths were recorded (cancer, 624; cardiovascular, 529; other causes, 811). Disparities in all-cause and cancer-specific mortality were observed between non-Hispanic Black and White cancer survivors. Unemployment, lower economic status, education less than high school, government or no private insurance, renting a home or other arrangements, and social isolation were significantly and independently associated with worse overall survival. Unemployment, lower economic status, and social isolation were significantly associated with cancer-specific mortality. Compared to patients without an unfavorable SDoH, the risk of all-cause mortality was gradually increased in those with a cumulative number of unfavorable SDoHs (1 unfavorable SDoH: hazard ratio [HR] = 1.54, 95% CI 1.25–1.89; 2 unfavorable SDoHs: HR = 1.81, 95% CI 1.46–2.24; 3 unfavorable SDoHs: HR = 2.42, 95% CI 1.97–2.97; 4 unfavorable SDoHs: HR = 3.22, 95% CI 2.48–4.19; 5 unfavorable SDoHs: HR = 3.99, 95% CI 2.99–5.33; 6 unfavorable SDoHs: HR = 6.34 95% CI 4.51–8.90). A similar trend existed for cancer-specific mortality.
Conclusions
In this cohort study of a nationally representative sample of US cancer survivors, a greater number of unfavorable SDoH was associated with increased risks of mortality from all causes and cancer. Unfavorable SDoH levels were critical risk factors for all-cause and cancer-specific mortality, as well as the underlying cause of racial all-cause mortality disparities among US cancer survivors.
Background
An increase in the cancer survivor population poses a significant health care and economic burden worldwide, and cancer is the second leading cause of death in the United States (US). Specifically, there will be approximately 2,001,140 new cancer cases and an estimated 611,720 deaths from cancer in the US in 2024 [1]. Although cancer mortality has declined overall by 33% since 1991, improved survival outcomes have not benefitted equally for all cancer populations [1, 2]. Substantial racial and ethnic disparities in all-cause and cancer-related mortality rates persist in US cancer survivors [1,2,3,4]. For example, Black individuals have lower relative cancer survival rates than White individuals for almost every cancer type [1, 5]. Interestingly, the most striking gaps in survival involve cancers that are most amenable to prevention and early detection, such as cervical cancer [5]. Recently, the racial and ethnic disparities in cancer mortality have slowly narrowed; however, these disparities in cancer health have become increasingly understood in the context of social determinants of health (SDoH) [2, 5, 6], which are responsible for an extremely important factor associated with cancer risk and treatment [7]. The World Health Organization (WHO) defined SDoH as non-medical factors that affect health outcomes, including the conditions in which people are born, grow, live, work, and age, and a wider set of forces and systems shaping daily life conditions [8]. The SDoH included factors related to economic stability, education, health care access, residential environment, and social context and support [9,10,11], associated with the health outcomes of cancer survivors [12, 13]. Addressing social disparities in cancer health is essential in the quest to improve survival outcomes among cancer survivors, which reflects a commitment to health equity to achieve optimal health for everyone.
Previous studies have tended to examine the contribution of individual variables involving unfavorable SDoHs in the separate associations with mortality or morbidity, most of which focused on the direct and indirect influence of socioeconomic factors on the disparity in survival [9, 14,15,16,17,18,19,20,21,22,23]. Among the general population, a large multicohort study and meta-analysis with more than 1.7 million individuals from 7 WHO member countries reported that low socioeconomic status was associated with a 46% (95% CI, 39–53%) and 43% (95% CI, 34–52%) greater risk of all-cause and cancer mortality, respectively, compared to high socioeconomic status [15]. A low level of education, poverty, and a lack of health insurance coverage explain in part the continuous widening in mortality inequities across some adult sociodemographic groups in the US [14, 17, 20, 24]. Additionally, a recent analysis demonstrated that the cumulative SDoH count was associated with an increased premature mortality risk [25]. However, limited evidence has been reported on the effect of SDoH in cancer survivors. Although previous cohort studies have shown that disadvantaged SDoH are associated with poor mental and physical health [26], resulting in a delay in medical and surgical treatment [27], and an increased risk of all-cause and cancer-related mortality among patients with cancers (such as breast and pancreatic cancer) [12, 13]. To the best of our knowledge, few studies have examined the impact of the comprehensive and accumulating burden of SDoH on all-cause and cause-specific mortality, using methods published previously [13, 25]. There is no study that has reported the relative contributions of these SDoH on racial disparities in the all-cause and cancer-specific mortality rates among the US cancer survivors at the population level.
The objective of the present study was to evaluate the relationships of multiple SDoH with all-cause, cancer-specific, and non-cancer mortality, and to investigate how SDoH mediates racial differences in all-cause and cancer-specific mortality among cancer survivors. We hypothesized that disparities exist in the cumulative number of unfavorable SDoH across racial and ethnic groups and that a higher number of these unfavorable SDoH is associated with higher mortality rates.
Methods
Study population
In this retrospective study, 10 cycles of cross-sectional data were collected from the National Health and Nutrition Examination Survey (NHANES) database, which used a complex, multistage, and probability sampling design to recruit participants representative of the civilian non-institutionalized US population [28]. Each participant was invited to attend an in-person or in-home interview to complete the questionnaire. The present study examined and analyzed existing data involving sociodemographic characteristics and several SDoH co-variables among cancer survivors of 20 years or older with information linked to the National Death Index through 31 December 2019 for 10 survey cycles of NHANES from 1999–2000 to 2017–2018. All the NHANES protocols were approved by the Research Ethics Review Board of the National Center for Health Statistics (NCHS), and written informed consent was provided by all participants at the time of recruitment.
Sociodemographic characteristics
In each 2-year survey, age, gender, and racial or ethnic groups (non-Hispanic White [NHW], Hispanic, non-Hispanic Black [NHB], and other [American Indian/Alaska Native/Pacific Islander, Asian, and multiracial]) were obtained from standardized questionnaires of in-home interviews by self or parent/guardian report from provided categories.
SDoH assessment
We included several variables that reflected SDoH information from standardized questionnaires, which were defined according to the Healthy People 2030 [11] and World Health Organization [29] by the following factors: economic stability; education access and quality; health access and quality; neighborhood and built environment; and social and community context. In the present study, we finally chose eight SDoH variables (employment status, family poverty income ratio, food security, education level, regular health care access, type of health insurance, home ownership, and marital status) in each NHANES cycles from 1999 to 2018, according to previously published studies [25, 30]. Social support was excluded because it was only visible in surveys conducted between 1999 and 2008. More detailed description information on SDoH was provided in the supplement (Additional file 1: Table S1) [31,32,33], and the definition for unfavorable SDoH was based on the conventional cutoff points [10, 11, 23, 34, 35]. Furthermore, the associations between several single SDoH measures and all-cause mortality were investigated using various categorizations with adjustment for age, gender, race, and ethnicity regardless of survey weights (Additional file 1: Table S2). Each SDoH was divided into two levels based on the conventional cut-off points [11, 23, 34, 35]. Unfavorable SDoH was significantly associated with a lower survival rate. During the in-person interview, participants were asked to respond to several questions about these SDoH. Economic stability was operationalized using self-reported measures of the family poverty income ratio (PIR, less than 2.4 [unfavorable SDoH] and more than 2.4 [favorable SDoH]), employment status (employed, student, or retired [favorable SDoH] and unemployed [unfavorable SDoH]) and household food security category, which was dichotomized as fully food security (no affirmative response) or marginal, low, or very low security (1–10 affirmative responses) based on the responses to the US Food Security Survey Module questions (Bickel et al. [36]). Education access and quality measurement used the highest grade or level of schooling completed or the highest degree received, dichotomized as less than high school (unfavorable SDoH) and high school graduate or higher (favorable SDoH). Health care access and quality were assessed by self-reported questionnaire about routine places for health care (at least one regular health care facility [favorable SDoH] and none or hospital emergency room [unfavorable SDoH]) and health insurance type (private [favorable SDoH] and none or government [unfavorable SDoH]). The residential environment was assessed by home ownership (owned or being bought [favorable SDoH] and rental or other arrangement [unfavorable SDoH]). Social community context was assessed by self-reported marital status (defined as married or living with a partner [favorable SDoH] and not married nor living with a partner [unfavorable SDoH]).
The cumulative number of unfavorable SDoH variables with a range from 0 (no unfavorable SDoH) to 6 or more (≥ 6 unfavorable SDoH) was calculated to explore the cumulative effect of unfavorable SDoH on all-cause and cancer-specific mortality. Because only a small proportion of participants reported having 6, 7, or 8 unfavorable SDoH variables simultaneously, thus we created a category of six or more, indicating the combination of 6, 7, or 8 unfavorable SDoH variables.
Definition of cancer survivors
Information on cancer diagnosis was collected from survey questionnaires during the in-person interview using the computer-assisted personal interview system, including cancer type(s), with up to three cancer diagnoses recorded and the age at first diagnosis for each cancer. Participants were asked, “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” If individuals who answered “yes” were defined as cancer survivors and were asked further, “What kind of cancer was it?” and “How old were you when this cancer was first diagnosed?”.
Ascertainment of mortality
The NCHS provided mortality data that were linked to the National Death Index, with follow-up until 31 December 2019 [37]. Cause-of-death coding for all US deaths occurring after 1998 followed the 10th revision of the International Statistical Classification of Diseases, Injuries, and Causes of Death (ICD-10) guidelines. Cancer-related mortality was classified as death due to malignant neoplasms (ICD-10, codes C00-C97). The follow-up duration was defined as the interval elapsing from the date of the baseline interview to the date of death or the follow-up cut-off (31 December 2019) for those participants who did not have a death event in the whole study. We investigated the association between SDoH and all-cause, cancer-related, and non-cancer mortality (mortality instead of cancer, ICD-10 codes instead of C00-97). All-cause and cancer-specific mortality were the main outcomes of this study. The all-cause mortality was measured from the date of the baseline interview to the date of death from any cause or the follow-up cut-off. The cancer-specific mortality was calculated from the date of the baseline interview to the date of death from cancer.
Statistical analysis
All statistical analyses were conducted with the use of R (version 4.3.1) following the NHANES analysis guidance. The survey interview weights were used for analysis as appropriate to obtain nationally representative estimates. We calculated weighted sample sizes to be nationally representative and population-weighted percentages according to race and ethnicity. The chi-square test was used to determine the differences in participants’ sociodemographic characteristics and SDoH variables across four classifications of racial and ethnic groups. The pairwise correlation among the eight dichotomous SDoH was evaluated using the Spearman method. The weighted proportions of cancer survivors in each number of unfavorable SDoH category were estimated by gender, race, and ethnicity. Kaplan–Meier survival curves were examined to determine the all-cause cumulative mortality and cancer-specific cumulative mortality rates among cancer survivors stratified by SDoH. Furthermore, Kaplan–Meier analysis was used to plot the cumulative hazard for all-cause and cancer-specific mortality in entire and gender subgroups and race and ethnicity subgroups using age as the timescale [38].
Multivariable Cox proportional hazards regression models with the use of imputation-adjusted survey weights were applied to estimate the mortality risks (hazard ratio [HR]) and 95% confidence interval (CI) for the associations between cumulative SDoH variables and race with all-cause, cancer-specific, and non-cancer mortality. Final stage multivariable Cox models were adjusted for age, gender, race, and ethnicity, and additionally included the other SDoHs to identify independent, indirect associations. We plotted the HRs of the cumulative SDoH variables to visualize whether the relationship with all-cause and cancer-specific mortality was linear or non-linear. Sensitivity analyses were performed by excluding participants of deaths that occurred within the first 2-year follow-up to lessen the probability of reverse causation [39]. All statistical tests were 2-sided and P < 0.05 was considered statistically significant. Data analyses were performed from 1 June to 1 August 2023.
Because of racial disparity in all-cause and cancer-specific mortality between NHW and NHB among cancer survivors in the US, therefore mediation analysis was performed to explore whether SDoH factors contributed to White-Black disparity in mortality or not. We estimated the relative effect (corresponding direct or indirect effect divided by the total effect) of each SDoH variable to explain the racial and ethnic difference in mortality using R package mma [31,32,33]. More detailed information was contained in the Supplementary material (Additional file 1: Methods S1).
Results
NHANES (1999–2018) data from 5163 individuals were enrolled in the final analysis (Additional file 1: Fig. S1). A total of 101,316 persons ≥ 1 year of age who participated in the in-person or in-home interview and 96,153 were excluded, as follows: (1) 46 235 participants < 20 years of age; (2) 49,915 whom were not diagnosed with cancer, and (3) 3 individuals who did not have unique identifiers to allow linkage to the National Death Index. Of the 5163 cancer survivors (weighted population, 32,623 176; 57.7% female) in this study cohort, 3580 (69.3%) were NHW, 631 (12.2%) were Hispanic, 718 (13.9%) were NHB, and 234 (4.5%) individuals of were classified as race and ethnicity, including American Indian/native Alaskan, Pacific Islander, Asian, and multiracial (Table 1). Compared to NHW, Hispanic, NHB and other race and ethnic cancer survivors were more likely to have unfavorable SDoH factors, including not being married nor living with a partner, education less than high school, a PIR < 2.4, renting a home or other arrangement, unemployment, government or none health insurance, and marginal, low, or very low security. However, a lower proportion of NHB participants had no place routine place when sick or in need of advice about healthcare compared with cancer survivors from all other racial and ethnic subgroups. Approximately 24.9% of cancer survivors did not have a cumulative number of unfavorable SDoH. The higher proportion of NHW cancer survivors with 0 and 1 cumulative unfavorable SDoH was observed compared to patients from all other race and ethnic subgroups. In addition, a higher proportion of Hispanic cancer survivors with 3, 4, 5, and 6 or more unfavorable SDoH was observed compared to patients from all other race and ethnic subgroups. NHB and Hispanic individuals had a higher prevalence of multiple unfavorable SDoH (cumulative of 3 or more) compared to NHW cancer survivors.
Then, we analyzed the relationship between the eight SDoH variables. The results showed that all eight SDoH variables were significantly correlated with each other (Additional file 1: Fig. S2). Furthermore, the proportion of male participants decreased stepwise from 34.8% (0 unfavorable SDoH) to 2.2% (6 or more number of unfavorable SDoH), whereas the proportion of female participants increased from 22.6% (0 unfavorable SDoH) to 24.8% (1 unfavorable SDoH), and then gradually decreased to 4.7% (6 or more number of unfavorable SDoH; Additional file 1: Fig. S3). Breast and prostate cancer were the most common malignant neoplasm type in males and females, respectively (Additional file 1: Table S3).
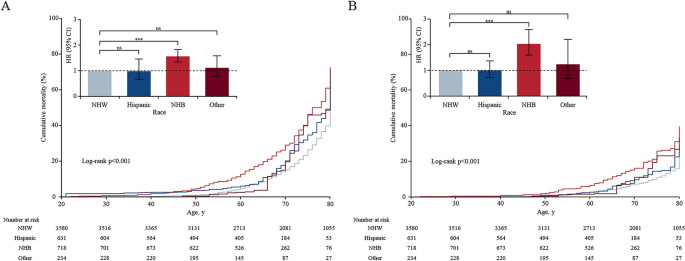
During the median follow-up of 81 months (ranged 0–249 months) in the 10 NHANES cycles linked mortality file cohort, a total of 1964 deaths occurred (all-cause), including 624 cancer patients who died from cancer (cancer-related mortality), 529 who died from cardiovascular disease, and 811 who died from other cause. Compared to participants who were NHW, NHB adults with cancer had a significantly higher overall mortality rate (HR, 1.57; 95% CI, 1.34–1.89) and cancer-specific mortality (HR, 2.03; 95% CI, 1.60–2.59; Fig. 1). Cancer survivors with each unfavorable SDoH variable, except access to regular health care, was significantly associated with higher all-cause, cancer-specific, and non-cancer mortality in the multivariable model adjusted for age (MV model 1), and adjusted for age, gender, race and ethnicity (MV model 2; Table 2). After adjustment for age, gender, race and ethnicity and other SDoHs, including unemployment status (HR, 1.83; 95% CI, 1.58–2.12; P < 0.001), family income-to-poverty less than 2.4 (HR, 1.51; 95% CI, 1.32–1.72; P < 0.001), education less than high school attached (HR, 1.23; 95% CI, 1.05–1.44; P = 0.012), government or none of health insurance (HR, 1.19; 95% CI, 1.05–1.36; P = 0.007), renting a home or other housing arrangement environment (HR, 1.39; 95% CI, 1.20–1.62; P < 0.001), and not being married nor living with a partner (HR, 1.22; 95% CI, 1.08–1.38; P < 0.001) were significantly associated with an increased risk for all-cause mortality, which was similar to non-cancer mortality (Table 2). Furthermore, unemployed individuals (HR, 2.13; 95% CI, 1.62–2.79; P < 0.001), family income-to-poverty less than 2.4 (HR, 1.35; 95% CI, 1.09–1.66; P = 0.006), and not being married nor living with a partner (HR, 1.22; 95% CI, 1.08–1.38; P < 0.001) were significantly associated with an increased cancer-specific mortality risk compared to those with favorable SDoH (Table 2). Specifically, individuals of being unemployed status were associated with almost more than 1.9- and 2.2-fold higher all-cause mortality and cancer-specific mortality rates, respectively.
All-cause mortality (A), cancer-specific mortality (B), and hazard ratios in US adults diagnosed with cancers aged 20 years or older by race and ethnicity. Note: Kaplan–Meier curves showed cumulative mortality probability race and ethnicity using age as the timescale. The number at risk was unweighted observed frequencies. Cumulative mortality rates were estimated with the use of survey weights. The bar chart showed HRs of all-cause and cancer-specific mortality associated with race and ethnicity, adjusted for age, and gender. Error bars were 95% CIs. NHW indicated non-Hispanic White; NHB indicated non-Hispanic Black; HR indicated hazard ratio; ns was the abbreviation of no significance; *** meant p < 0.001, ** meant p < 0.01, and * meant p < 0.05
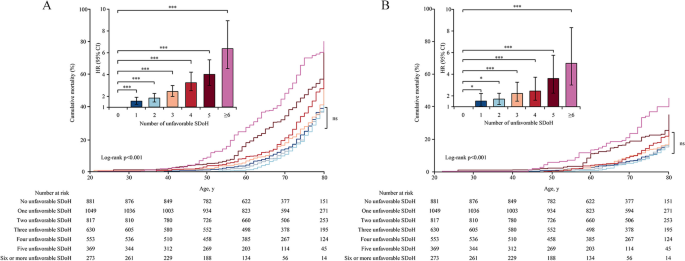
Cancer survivors with a greater cumulative number of SDoHs were significantly associated with an increased risk of death from all-cause and cancer (Additional file 1: Fig. S4; P < 0.001). In the multivariable of MV model 1 (adjusted for age, gender, race, and ethnic), the HRs for all-cause and cancer-specific mortality were 1.54 (95% CI, 1.25–1.89) and 1.52 (95% CI, 1.04–2.22) for cancer survivors with 1 unfavorable SDoH, 1.81 (95% CI, 1.46–2.24) and 1.70 (95% CI, 1.20–2.24) for those with 2 unfavorable SDoHs, 2.42 (95% CI, 1.97–2.97) and 2.22 (95% CI, 1.51–3.26) for those with 3 unfavorable SDoHs, 3.22 (95% CI, 2.48–4.19) and 2.44 (95% CI, 1.60–3.72) for those with 4 unfavorable SDoHs, 3.99 (95% CI, 2.99–5.33) and 3.60 (95% CI, 2.25–5.75) for those with 5 unfavorable SDoHs, and 6.34 (95% CI, 4.51–8.90) and 5.00 (95% CI, 3.00–8.31) for those with 6 or more unfavorable SDoHs, respectively, compared with of whom without unfavorable SDoH (Fig. 2). Kaplan–Meier curves were used to estimate the cumulative probability of all-cause and cancer-specific mortality using age as the timescale. The all-cause and cancer-specific mortality rates were significant across the several groups with a cumulative number of unfavorable SDoHs (Fig. 2, P < 0.001). Pairwise comparison using log-rank showed that the all-cause mortality rate was similar and not significantly different among cancer survivors with 0, 1, 2, and 3 cumulative number of unfavorable SDoH across the entire age cohort (Additional file 1: Table S4). There was no significant difference in cancer-specific mortality among cancer survivors with 0, 1, 2, 3, and 4 cumulative number of unfavorable SDoH (Additional file 1: Table S5). Based on the linear dose–response analysis fitted curves (unfavorable SDoH ranged from 0 to 8), every cumulative unfavorable SDoH increase was significantly associated with 64% increased risks of death from all-cause (HR per 1-number increase, 1.64 [95% CI, 1.50–1.78]), and 53% of cancer (HR per 1-number increase, 1.53 [95% CI, 1.45–1.60]) (Additional file 1: Fig. S5 and Table 2; P < 0.001 for linear trend).
All-cause mortality (A), cancer-specific mortality (B), and hazard ratios in US adults diagnosed with cancer aged 20 years or older according to the cumulative number of unfavorable SDoH. Note: Kaplan–Meier curves showed cumulative mortality probability by age and a cumulative number of unfavorable SDoH using age as the timescale. The number at risk is unweighted observed frequencies. Cumulative mortality rates were estimated with the use of survey weights. Bar chart showed hazard ratios of all-cause mortality and cancer-specific mortality associated with a number of unfavorable SDoH, adjusted for age, gender, and race and ethnicity; error bars were 95% CIs. A Compared to those with 0 unfavorable SDoH, all-cause mortality of hazard ratios (95% CI) for cancer survivors with 1, 2, 3, 4, 5, or ≥ 6 unfavorable SDoH were 1.54 (1.25–1.89), 1.81 (1.46–2.24), 2.42 (1.97–2.97), 3.22 (2.48–4.19), 3.99 (2.99–5.33), and 6.34 (4.51–8.90), respectively. B Compared to those with 0 unfavorable SDoH, cancer-specific mortality of hazard ratios (95% CI) for cancer survivors with 1, 2, 3, 4, 5, or ≥ 6 unfavorable SDoH were 1.52 (1.04–2.22), 1.70 (1.20–2.24), 2.22 (1.51–3.26), 2.44 (1.60–3.72), 3.60 (2.25–5.75), and 5.00 (3.00–8.31), respectively. ns was the abbreviation of no significance; *** meant p < 0.001, ** meant p < 0.01, and * meant p < 0.05
Age-adjusted/ age-gender-adjusted all-cause mortality and cancer-specific mortality risk were significantly higher in NHB cancer survivors when compared with NHW. Further adjustment for all SDoH factors, black-white disparity in cancer-specific mortality was still observed (HR 1.45, 95% CI 1.07–1.96), and the all-cause mortality did not show a statistically significant difference (HR, 1.08; 95% CI 0.89–1.30; Table 3). In the mediation analysis, the socioeconomic factor of unemployment (17.5% for all-cause mortality; 15.3% for cancer-specific mortality) can mostly explain the racial disparity in all-cause and cancer-specific mortality, and unemployment was associated with a nearly 90% and 120% greater all-cause and cancer-specific mortality, respectively. A family income-to-poverty ratio less than 2.4 (15.7%), an education less than high school (8.1%), government health insurance (6.9%), renting a home or other housing arrangement (15.4%), and not being married nor living with a partner (13.4%) indicated effective relative contribution to the disparity of all-cause mortality between NHB and NHW cancer survivors. An additional factor (not being married nor living with a partner [10.2%]) contributed significantly to the racial difference in cancer-specific mortality (Table 3).
In the subgroup analysis, NHW cancer survivors who were unemployed, a lower level of PIR, an education less than high school, government or none of health insurance, renting a home or other housing arrangement, and not being married nor living with a partner were significantly more likely to die of all-cause mortality compared to NHW cancer survivors without unfavorable SDoH. Unemployment and not being married nor living with a partner were significantly associated with a higher risk of cancer-specific mortality (Additional file 1: Table S6). Being unemployed and having no access to a regular health care facility or emergency room was significantly associated with all-cause mortality in NHB cancer survivors. Only unemployed status was associated with cancer-specific mortality (Additional file 1: Table S6). In the stratified analysis by gender (female and male), almost all unfavorable SDoH were significantly associated with greater all-cause and cancer-specific mortality for female and male subgroups after adjusting for age, except for cancer-specific mortality for unfavorable home ownership (Additional file 1: Table S7). In all sensitivity analyses excluding mortalities that happened during the first 2-year follow-up since the baseline interview, all results remained similar in association with unfavorable SDoH with all-cause, cancer-specific, and non-cancer mortality (Additional file 1: Table S8).
In this US nationally representative cohort study of cancer survivors, we found that NHB and Hispanic adult cancer survivors self-reported a higher proportion of multiple unfavorable SDoHs compared to NHW adults diagnosed with cancer. Compared to NHW cancer survivors, NHB cancer survivors had significantly higher all-cause and cancer-specific mortality after adjusting for age and gender. In addition, after further adjusting for all SDoH, there was no longer a difference between NHB and NHW cancer survivors in all-cause mortality, but a significant difference in cancer-specific mortality was still observed. These findings suggest that racial differences in all-cause mortality between NHW and NHB cancer survivors were largely attributable to the explained by differences in SDoH, while cancer-specific mortality disparities were partly explained by differences in SDoH. Furthermore, unfavorable SDoH were associated with a higher risk of all-cause and cancer-specific mortality for cancer survivors. During the 20 years of follow-up, an increasing number of unfavorable SDoHs in the same individual was associated with an increased risk of dying from all causes, cancer, and noncancer causes, even after adjusting for demographic factors, such as age, gender, and race. Of note, there were significantly linear dose–response relationships between the cumulative number of unfavorable SDoHs and all-cause and cancer-specific mortality among cancer survivors, and cancer survivors having six or more unfavorable SDoH increased the HR for mortality of 6.34 and 5.00 compared to those having no unfavorable SDoH, respectively.
NHB cancer survivors were more likely than NHW patients to have unfavorable levels of all SDoH. Compared to NHW cancer survivors, NHB and Hispanic cancer survivors were 3.0 times and 3.9 times more likely to experience six or more unfavorable SDoHs, respectively, which may partly explain the racial disparity in mortality. Most predominantly, NHB cancer survivors were 1.6 times more likely than NHW cancer survivors to have family PIR less than 2.4, which was associated with almost 50% and 25% greater all-cause mortality and cancer-specific mortality, respectively. Most recently, Connolly et al. [30] conducted a study involving a cohort of 3590 participants from NHANES between 1999 and 2014, and demonstrated that the SDoH level was more favorable for NHW compared to NHB adolescents. Our finding was consistent with another previous study that reported a lower level of PIR, lower level of education attachment, lack of health insurance coverage, dietary insecurity, and limited health access were more common in NHB compared to NHW, which was a key mediator in explaining race disparity in all-cause and cause-specific mortality, especially cardiovascular disease and neoplasms [17, 40].
The persistent disparities in survival by race and ethnicity among cancer patients have been well-documented [2,3,4, 6, 41], and these disparities between NHB and NHW cancer survivors were particularly stark [42]. Indeed, the overall cancer mortality in 2022 for male and female together was 12% (166.8 vs. 149.3 per 100,000 persons, respectively) higher in NHB compared to NHW cancer survivors [6]. However, racial differences were not the only factor that contributed to observed mortality disparity and the underlying causes attributed to these disparities have not been well established [43]. Various factors have been suggested as contributors to these racial and ethnic disparities in survival outcomes among cancer survivors, including differences in tumor characteristics [44, 45], neighborhood socioeconomic deprivation [42], and accessibility to health care. In the current study, disparities in the all-cause mortality HR for NHB cancer survivors compared to NHW cancer survivors decreased from 1.59 (95% CI, 1.36–1.86) to 1.09 (95% CI, 0.91–1.31) after adjusting for all SDoHs, which mostly mediated the racial disparity in all-cause mortality. With respect to cancer-specific mortality, the HR for NHB cancer survivors compared to NHW cancer survivors decreased from 2.04 (95% CI, 1.60–2.62) to 1.45 (95% CI, 1.07–1.96) after adjusting for all SDoHs, which has a partly mediator role in the racial difference. We found that cancer survivors with employed, student or retired status (17.5% relative contribution), and PIR more than 2.4 (15.7% relative contribution) explained the greatest percentage of disparities in all-cause mortality. Furthermore, we also showed that employed, student, or retired status (15.3% relative contribution) and being married or living with a partner (10.2% relative contribution) explained the largest portions of disparities in cancer-specific mortality. Taken together, the traditional socioeconomic factors consisting of household income, level of education completed, and unemployment status were important explanatory factors, that mediated around 45% and 25% of all-cause and cancer-specific mortality in survival inequities between NHB and NHW cancer survivors, respectively, which was consistent with the findings of Bundy et al. (nearly 50% mediated the differential in all-cause premature mortality) [25]. The SDoH, through an impact on occupational opportunities and income levels, have a substantial influence on insurance coverage, which was one of the main factors determining access to and delivery of health care services in the US as well as associated disparities in survival [40]. Conversely, these traditional economic factors have a greater effect on the racial/ethnic disparities in the general population compared to cancer patients. Specifically, Luo et al. [20] suggested that income mediated 62% of the association in mortality between NHB and NHW, which was consistent with the dominant contributors to family income (40%) and education (19%) to the gap between NHB and NHW adult populations [17]. Interestingly, NHW cancer survivors were approximately 25% more likely to be married or living with a partner compared to NHB cancer survivors. Being married or living with a partner was associated with the cancer-related survival benefits, possibly due to increased social support and higher psychological well-being and instrumental support, helping navigate the health care system [46, 47]. According to Fuzzel et al. [48], barriers to health care accessibility and insurance coverage have a significant impact on rates of cancer screening, as well as the burden and attributions of the disease. These findings suggested SDoH factors, as an important mediator, drive racial health disparities, as well as all-cause and cancer-specific mortality, highlighting the necessity of the level of SDoH contexts for all people, especially those who are more vulnerable to unfavorable SDoH.
The cumulative adverse SDoHs were associated with poor all-cause survival and cause-specific survival rates among the cancer-free population have been previously reported, e.g., among patients with cardiovascular disease. Sameroff et al. [49] reported that cumulative unfavorable social risk factors, such as food insecurity combined with social isolation and loneliness, have a higher relevance to poor health outcomes than single social risk factors. Jilani et al. [50] suggested that greater SDoH adversity was linked to a higher burden of cardiovascular risk factors and poor health outcomes, such as stroke, myocardial infarction, coronary heart disease, heart failure, and mortality. Similarly, Zhang et al. [16] combined family income level, occupation, education level, and health insurance to measure socioeconomic status, and reported that participants who met low socioeconomic status had higher risks of all-cause mortality (HR, 2.13 and 95% CI, 1.90–2.38 in the US NHANES; HR, 1.96 and 95% CI, 1.87–2.06 in the UK Biobank), cardiovascular disease mortality (HR, 2.25; 95% CI, 2.00–2.53), and incident cardiovascular disease (HR, 1.65; 95% CI, 1.52–1.79) in UK Biobank, compared to high socioeconomic status. Our results were consistent with the findings of a study in which each additional SDoH conferred additional cancer-related mortality, compared to cancer survivors without any SDoH (1 SDoH [HR, 1.39; 95% CI, 1.11–1.75], 2 SDoHs [HR, 1.61; 95% CI, 1.26–2.07], and ≥ 3 SDoHs [HR, 2.09; 95% CI, 1.58–2.75]) [13]. In contrast, Weires et al. [51] observed that women with a higher socioeconomic status showed increased mortality due to breast cancer in Sweden. This finding may be due to the structure of the Swedish family cancer database (Swedes born after 1931 and their biological parents), as well as analytical restrictions on individuals 30–60 years of age in 1960, which may exclude low-socioeconomic adults with severe health problems. Previous studies have shown that these unfavorable SDoH have a tendency to cluster in individuals [13, 23]. For example, individuals in the general US population who self-reported food insecurity were more likely to be combined with a low level of education attachment, not being married, a low level of family income, and a bad lifestyle. This finding was consistent with our observation that these unfavorable SDoH were not isolated but interrelated, and each unfavorable SDoH included in our study has been found to independently increase the risk of mortality. Compared to most previous studies based on a single SDoH, we found that there was a simple linear dose–response relationship reflecting the cumulative effect of multiple unfavorable SDoHs on all-cause and cancer-specific mortality. Collectively, these SDoH appear to synergistically increase the risk of all-cause and cancer-specific mortality among cancer survivors. However, the cumulative risk derived from a sum of the number of unfavorable SDoH assumed that all SDoH had equal and independent effects on survival outcomes, which might not be precise. We suggest that future research may need to use more complex models, such as interaction models, to more accurately capture the complex interactions of unfavorable SDoH.
Strengths and limitations
The major strength of this study was the use of large sample size data from the NHANES, which provides an opportunity to comprehensively evaluate the complex relations of SDoH with all-cause and cancer-specific mortality among cancer survivors. In addition, we focused on multiple SDoH factors and estimated the effect of accumulating unfavorable SDoH burden on mortality. We also performed mediation analysis to show the contribution of SDoH to disparities in all-cause and cancer-specific mortality. There were some limitations in the present study. First, we conducted the analyses based on the follow-up of time-to-event, however, all data on SDoH variables were only assessed at the baseline interview, which may not reflect factors that changed during the follow-up period. Therefore, our study was not able to quantify the effect of changes in eight SDoH on the mortality of cancer survivors over time. It is essential to conduct several repeated interviews about the level of SDoH during the follow-up period to reveal the influence of SDoH factors on survival among cancer survivors. Second, the assessment of SDoH was limited by the availability of variables in the NHANES database. Some SDoH such as neighborhood environment, social support, and exposure to racism, were not widely available, which may also contribute to the all-cause and cancer-specific mortality. Third, the follow-up duration was relatively short (median, 81 months) and an important bias among these cancer survivors such that socially disadvantaged who died during the study period might have had severe disease at baseline.
Conclusions
In conclusion, in this cohort study of a nationally representative sample of US cancer survivors between 1999 and 2018, there were significant differences in SDoH and mortality rates across self-reported racial and ethnic groups. Unfavorable SDoH were more common among NHB cancer survivors than NHW cancer survivors, were strongly associated with an increased risk of all-cause and cancer-specific mortality, and largely explained the difference between NHB and NHW cancer survivors in all-cause mortality, as well as partially explained these racial disparities in cancer-specific mortality. In addition, the cancer participants with a greater cumulative number of unfavorable SDoHs also appeared to be associated with higher risks of death from all-causes, and cause-specific (cancer and non-cancer). Taken together with previous findings, the unfavorable SDoH levels were the major risk factors for all-cause and cancer-specific mortality and were the underlying causes in all-cause racial health disparities among US cancer survivors. The entire government, civil society, local communities, businesses, and international agencies must pay more attention to the upstream SDoH, such as economic resources, employment, education quality, and racial discrimination [52]. We believe that these findings shed highlight on the cumulative burden of SDoHs on all-cause and cancer-specific mortality among cancer survivors, providing insight for ongoing and future initiatives aimed at mitigating mortality rates within vulnerable populations, including racial/ethnic minorities and individuals with an unfavorable level of SDoH status. Addressing social disparities in cancer health is a very important part of improving survival outcomes for cancer survivors, reflecting a commitment to health equity—aimed at achieving the optimal health for everyone.
Availability of data and materials
The US NHANES are publicly available database and all data can be accessed from https://wwwn.cdc.gov/nchs/nhanes/. The statistical code and data required to reproduce the results presented in this article can be requested from Hongbo Huang (2023150448@stu.cqmu.edu.cn) or Fan Li (lf628@163.com).
Abbreviations
- SDoH:
-
Social determinants of health
- WHO:
-
World Health Organization
- NCHS:
-
National Center for Health Statistics
- ICD:
-
International Statistical Classification of Diseases, Injuries, and Causes of Death
- NHW:
-
Non-Hispanic White
- NHB:
-
Non-Hispanic Black
- HR:
-
Hazard ratio
- NHANES:
-
National Health and Nutrition Examination Survey
- US:
-
United States
References
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12–49.
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: A blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31–46.
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, Jemal A, Kramer JL, Siegel RL. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85.
Kurani SS, McCoy RG, Lampman MA, Doubeni CA, Finney Rutten LJ, Inselman JW, Giblon RE, Bunkers KS, Stroebel RJ, Rushlow D, et al. Association of Neighborhood Measures of Social Determinants of Health With Breast, Cervical, and Colorectal Cancer Screening Rates in the US Midwest. JAMA Netw Open. 2020;3(3).
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48.
Yu Z, Yang X, Guo Y, Bian J, Wu Y. Assessing the Documentation of Social Determinants of Health for Lung Cancer Patients in Clinical Narratives. Front Public Health. 2022;10.
World Health Organization. Social determination of health. [https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1].
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129 Suppl 2(Suppl 2):19–31.
A conceptual framework for action on the social determinants of health. [https://iris.who.int/handle/10665/44489].
U.S Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2030: Social Determinants of Health. [https://health.gov/healthypeople/priority-areas/social-determinants-health].
Fabregas JC, Riley KE, Brant JM, George TJ, Orav EJ, Lam MB. Association of social determinants of health with late diagnosis and survival of patients with pancreatic cancer. J Gastrointest Oncol. 2022;13(3):1204–14.
Pinheiro LC, Reshetnyak E, Akinyemiju T, Phillips E, Safford MM. Social determinants of health and cancer mortality in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study. Cancer. 2022;128(1):122–30.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D. The Association Between Income and Life Expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–66.
Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, Ricceri F, d’Errico A, Barros H, Bochud M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389(10075):1229–37.
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, Liu G, Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604.
Beydoun MA, Beydoun HA, Mode N, Dore GA, Canas JA, Eid SM, Zonderman AB. Racial disparities in adult all-cause and cause-specific mortality among us adults: mediating and moderating factors. BMC Public Health. 2016;16(1):1113.
Braveman PA, Egerter SA, Cubbin C, Marchi KS. An approach to studying social disparities in health and health care. Am J Public Health. 2004;94(12):2139–48.
Meneton P, Kesse-Guyot E, Méjean C, Fezeu L, Galan P, Hercberg S, Ménard J. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health. 2015;88(6):707–16.
Luo J, Hendryx M, Wang F. Mortality disparities between Black and White Americans mediated by income and health behaviors. SSM Popul Health. 2022;17:101019.
Petrovic D, de Mestral C, Bochud M, Bartley M, Kivimäki M, Vineis P, Mackenbach J, Stringhini S. The contribution of health behaviors to socioeconomic inequalities in health: A systematic review. Prev Med. 2018;113:15–31.
Sun Y, Liu B, Rong S, Du Y, Xu G, Snetselaar LG, Wallace RB, Bao W. Food Insecurity Is Associated With Cardiovascular and All-Cause Mortality Among Adults in the United States. J Am Heart Assoc. 2020;9(19):e014629.
Walker RJ, Chawla A, Garacci E, Williams JS, Mendez C, Ozieh MN, Egede LE. Assessing the relationship between food insecurity and mortality among U.S. adults. Ann Epidemiol. 2019;32:43–8.
Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329(2):103–9.
Bundy JD, Mills KT, He H, LaVeist TA, Ferdinand KC, Chen J, He J. Social determinants of health and premature death among adults in the USA from 1999 to 2018: a national cohort study. Lancet Public Health. 2023;8(6):e422–31.
Su LJ, O’Connor SN, Chiang TC. Association Between Household Income and Self-Perceived Health Status and Poor Mental and Physical Health Among Cancer Survivors. Front Public Health. 2021;9:752868.
Neroda P, Hsieh MC, Wu XC, Cartmell KB, Mayo R, Wu J, Hicks C, Zhang L. Racial Disparity and Social Determinants in Receiving Timely Surgery Among Stage I-IIIA Non-small Cell Lung Cancer Patients in a U.S. Southern State. Front Public Health. 2021;9:662876.
Centers for Disease Control and Prevention. National Center for Health Statistics. National Health and Nutrition Examination Survey. [https://wwwn.cdc.gov/nchs/nhanes/].
Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–9.
Connolly SD, Lloyd-Jones DM, Ning H, Marino BS, Pool LR, Perak AM. Social Determinants of Cardiovascular Health in US Adolescents: National Health and Nutrition Examination Surveys 1999 to 2014. J Am Heart Assoc. 2022;11(22):e026797.
Yu Q, Li B. mma: an R package for mediation analysis with multiple mediators. J Open Res Software. 2017. https://doi.org/10.5334/jors.160.
Yu Q, Scribner RA, Leonardi C, Zhang L, Park C, Chen L, Simonsen NR. Exploring racial disparity in obesity: A mediation analysis considering geo-coded environmental factors. Spat Spatiotemporal Epidemiol. 2017;21:13–23.
Yu Q, Wu X, Li B, Scribner RA. Multiple mediation analysis with survival outcomes: With an application to explore racial disparity in breast cancer survival. Stat Med. 2019;38(3):398–412.
Gómez CA, Kleinman DV, Pronk N, Wrenn Gordon GL, Ochiai E, Blakey C, Johnson A, Brewer KH. Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. J Public Health Manag Pract. 2021;27(Suppl 6):S249-s257.
He J, Zhu Z, Bundy JD, Dorans KS, Chen J, Hamm LL. Trends in Cardiovascular Risk Factors in US Adults by Race and Ethnicity and Socioeconomic Status, 1999–2018. JAMA. 2021;326(13):1286–98.
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security : revised March, 2000. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. March; 2000.
National Center for Health Statistics. 2019 Public-Use Linked Mortality Files. [https://www.cdc.gov/nchs/data-linkage/mortality-public.htm].
Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145(1):72–80.
Sattar N, Preiss D. Reverse Causality in Cardiovascular Epidemiological Research: More Common Than Imagined? Circulation. 2017;135(24):2369–72.
Islami F, Guerra CE, Minihan A, Yabroff KR, Fedewa SA, Sloan K, Wiedt TL, Thomson B, Siegel RL, Nargis N, et al. American Cancer Society’s report on the status of cancer disparities in the United States, 2021. CA Cancer J Clin. 2022;72(2):112–43.
Aizer AA, Wilhite TJ, Chen MH, Graham PL, Choueiri TK, Hoffman KE, Martin NE, Trinh QD, Hu JC, Nguyen PL. Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period. Cancer. 2014;120(10):1532–9.
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Racial and Ethnic Disparities in Cancer Survival: The Contribution of Tumor, Sociodemographic, Institutional, and Neighborhood Characteristics. J Clin Oncol. 2018;36(1):25–33.
Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C. In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. edn. Edited by Smedley BD, Stith AY, Nelson AR. Washington (DC): National Academies Press (US). Copyright 2002 by the National Academy of Sciences. All rights reserved. 2003.
Özdemir BC, Dotto GP. Racial Differences in Cancer Susceptibility and Survival: More Than the Color of the Skin? Trends Cancer. 2017;3(3):181–97.
Virnig BA, Baxter NN, Habermann EB, Feldman RD, Bradley CJ. A matter of race: early-versus late-stage cancer diagnosis. Health Aff (Millwood). 2009;28(1):160–8.
Gomez SL, Hurley S, Canchola AJ, Keegan TH, Cheng I, Murphy JD, Clarke CA, Glaser SL, Martínez ME. Effects of marital status and economic resources on survival after cancer: A population-based study. Cancer. 2016;122(10):1618–25.
Pinquart M, Duberstein PR. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol. 2010;75(2):122–37.
Fuzzell LN, Perkins RB, Christy SM, Lake PW, Vadaparampil ST. Cervical cancer screening in the United States: Challenges and potential solutions for underscreened groups. Prev Med. 2021;144:106400.
Sameroff AJ, Rosenblum KL. Psychosocial constraints on the development of resilience. Ann N Y Acad Sci. 2006;1094:116–24.
Jilani MH, Javed Z, Yahya T, Valero-Elizondo J, Khan SU, Kash B, Blankstein R, Virani SS, Blaha MJ, Dubey P, et al. Social Determinants of Health and Cardiovascular Disease: Current State and Future Directions Towards Healthcare Equity. Curr Atheroscler Rep. 2021;23(9):55.
Weires M, Bermejo JL, Sundquist K, Sundquist J, Hemminki K. Socio-economic status and overall and cause-specific mortality in Sweden. BMC Public Health. 2008;8:340.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98.
Acknowledgements
We thank Dr Jing Yi (School of Public Health, Chongqing Medical University, Chongqing, 400016, China) for suggestions on the used in mediation analysis and International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Funding
This study was supported by grant 82202913 (Dr Yunhai Li) and 82372996 (Dr Fan Li) from the National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
HBH, YHL and FL designed the study. HBH, YHL, TTW, and YH conducted the statistical analyses. HBH, TTW, YH, AJZ, ZZ, HZ, YJX, HNP, YHL, and FL drafted the original manuscript. HBH, YHL, LQK and FL review the manuscript. All authors approved the final version of manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The US NHANES database has been approved by the National Center for Health Statistics Ethics Review Board (https://www.cdc.gov/nchs/nhanes/irba98.htm), and written informed consent was provided by all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12916_2024_3563_MOESM1_ESM.docx
Additional files 1: Method S1. Details about mediation analysis. Table S1. SDoH based on the Office of Disease Prevention and Health Promotion’s Healthy People 2030 and World Health Organization in NHANES 1999–2018. Table S2. Candidate social determinants of healthand associations with all-cause mortality in the US cancer survivors, NHANES 1999–2018. Table S3. Number of cancer survivor by cancer type and gender, NHANES 1999–2018. Table S4. P value for overall survival outcomes pairwise comparisons using log-rank test with Bonferroni adjustment. Table S5. P value for cancer-specific survival outcomes pairwise comparisons using log-rank test with Bonferroni adjustment. Table S6. Associations of social determinants of healthwith all-cause and cancer-specific mortality in US cancer survivors by race/ethnicity, NHANES 1999–2018. Table S7. Associations of social determinants of healthwith all-cause and cancer-specific mortality in US cancer survivors by gender, NHANES 1999–2018. Table S8. Sensitivity analyses of association social determinants of healthand all-cause, cancer-specific and non-cancer mortality in weighted and fully adjusted multivariable analysis among cancer survivors, NHANES 1999–2018. Fig. S1 Flowchart of participants selection for current analysis from NHANES 1999–2018. Fig. S2 The pairwise correlation between social determinants of healthusing Spearman method. Fig. S3 The proportion for each cumulative number of social determinants of healthby gender. Fig. S4 All-cause mortalityand cancer-specific mortalityfor cancer survivors aged 20 years or older in US between 1999 and 2018 stratified by cumulative number of unfavorable social determinants of health. Fig. S5 Linear dose–response association between cumulative number of unfavorable social determinants of healthand all-cause of death, and cancer deathamong US cancer survivors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, H., Wei, T., Huang, Y. et al. Association between social determinants of health and survival among the US cancer survivors population. BMC Med 22, 343 (2024). https://doi.org/10.1186/s12916-024-03563-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03563-0