- Research article
- Open access
- Published:
NHS Health Check attendance is associated with reduced multiorgan disease risk: a matched cohort study in the UK Biobank
BMC Medicine volume 22, Article number: 1 (2024)
Abstract
Background
The NHS Health Check is a preventive programme in the UK designed to screen for cardiovascular risk and to aid in primary disease prevention. Despite its widespread implementation, the effectiveness of the NHS Health Check for longer-term disease prevention is unclear. In this study, we measured the rate of new diagnoses in UK Biobank participants who underwent the NHS Health Check compared with those who did not.
Methods
Within the UK Biobank prospective study, 48,602 NHS Health Check recipients were identified from linked primary care records. These participants were then covariate-matched on an extensive range of socio-demographic, lifestyle, and medical factors with 48,602 participants without record of the check. Follow-up diagnoses were ascertained from health records over an average of 9 years (SD 2 years) including hypertension, diabetes, hypercholesterolaemia, stroke, dementia, myocardial infarction, atrial fibrillation, heart failure, fatty liver disease, alcoholic liver disease, liver cirrhosis, liver failure, acute kidney injury, chronic kidney disease (stage 3 +), cardiovascular mortality, and all-cause mortality. Time-varying survival modelling was used to compare adjusted outcome rates between the groups.
Results
In the immediate 2 years after the NHS Health Check, higher diagnosis rates were observed for hypertension, high cholesterol, and chronic kidney disease among health check recipients compared to their matched counterparts. However, in the longer term, NHS Health Check recipients had significantly lower risk across all multiorgan disease outcomes and reduced rates of cardiovascular and all-cause mortality.
Conclusions
The NHS Health Check is linked to reduced incidence of disease across multiple organ systems, which may be attributed to risk modification through earlier detection and treatment of key risk factors such as hypertension and high cholesterol. This work adds important evidence to the growing body of research supporting the effectiveness of preventative interventions in reducing longer-term multimorbidity.
Background
With ageing populations globally, the increasing multimorbidity burden is having a serious impact on healthcare costs, disability, and mortality [1]. Although multimorbidity prevention is now recognised as a high priority [2], and forms part of the National Health Service (NHS) Long Term Plan [3], there are few established strategies with known effectiveness. Disease prevention is particularly challenging when conditions develop over a long period of time without symptoms, meaning that disease is often only detected once it has progressed to advanced stages. Therefore, when it comes to multimorbidity prevention, a proactive—rather than reactive—approach may be required [4].
The NHS Health Check programme is a preventative primary care intervention launched in England, UK, in 2009, designed to identify individuals at risk for heart disease, stroke, diabetes, and kidney disease [5, 6]. Briefly, under the NHS Health Check protocol, healthy adults aged 40–74 are invited to visit their primary care team for basic physical checks, blood tests, and health behaviour questions, after which attendees are offered support and services to help prevent or delay the onset of these conditions. With a similar and slightly expanded protocol, the Scottish version (“Keep Well”) was launched in 2006 and is specifically targeted towards areas of socio-economic deprivation [7, 8].
There is a growing body of evidence around the administration and uptake of the NHS Health Check [9, 10]. However, there is much less research on the associations between NHS Health Check and subsequent health outcomes and the effectiveness of the programme in disease prevention. Although there is some existing work documenting the short-term effects of NHS Health Check [11, 12], evidence regarding longer-term outcomes is proving to be particularly challenging to find. Additionally, the evidence we have often fails to account for follow-up outcomes across multiple disease endpoints. Preventive public health programmes are also in place in other nations [13, 14]; however, similar gaps in evidence exist in relation to the value of such strategies in promoting long-term health.
In this study, we draw upon the UK Biobank resource to identify participants who have received an NHS Health Check and to observe any new diagnoses received during the follow-up period. The objective of this study is to compare the health outcomes across multiple morbidities, in participants with and without evidence of receiving an NHS Health Check.
Methods
This is an observational, case–control study reported in accordance with the STROBE guidelines (see Additional file 1: Checklist S1).
Study sample
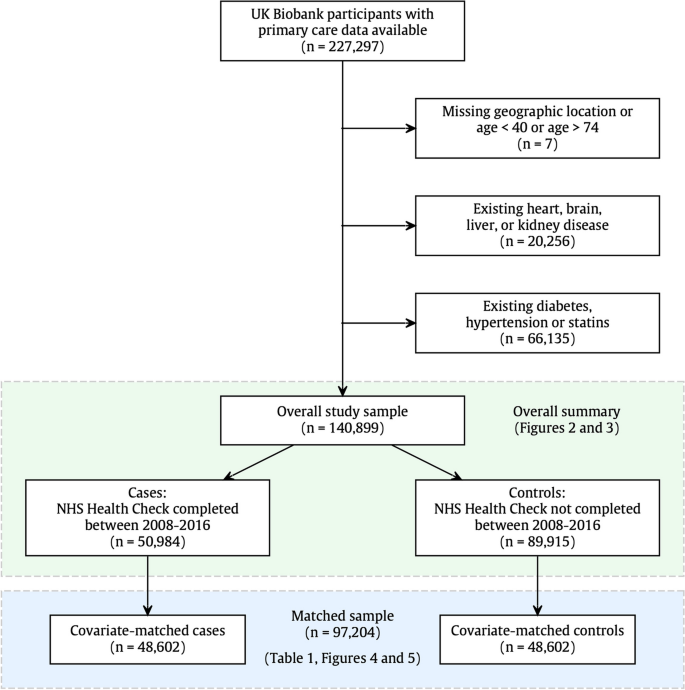
The UK Biobank is a UK-wide prospective cohort study, with baseline recruitment taking place between March 2006 and October 2010. At the time of this study, there were 227,297 participants who had completed consent for their primary care records to be made available and who had confirmed primary care records in the database (Fig. 1). From this pool of participants, 7 participants had missing geographical location or were outside the age range for the NHS Health Check. A further 20,256 participants (9%) were excluded as ineligible for an NHS Health Check due to an existing diagnosis of heart, brain, liver, or kidney disease, and 66,135 participants (31%) were excluded due to statins prescription or an existing diagnosis of diabetes or hypertension. The NHS Health Check criteria specifically exclude people with these conditions as they are considered to be already identified and managed by their NHS providers. Thus, 140,899 participants were used as the study sample.
Study sample selection. Inclusion for this study was dependent on participants having primary care data available and eligibility for the NHS Health check. In other words, participants were between 40 and 74 years and had no existing diagnoses that would normally mean regular primary care monitoring. Overall summaries in Figs. 2 and 3 relate to the full study sample (n = 140,899), and outcome modelling was performed with the covariate-matched sample (n = 97,204), with details shown in Table 1 and Figs. 4 and 5
Case–control matching
In order to reduce confounding from known sources, we applied an extensive case–control matching algorithm, to produce a control group that was matched one-to-one with NHS Health Check recipients using nearest neighbour propensity score matching with a calliper width of 0.2, as per published recommendations [15]. Matching was conducted with respect to demographic features (geographical region, age, sex, ethnicity, Townsend deprivation index, education), family history of disease (stroke, heart disease, dementia), physical measures (body mass index, waist-to-hip ratio, systolic blood pressure at baseline), and health behaviours (smoking, alcohol intake frequency, physical activity, and daily vegetable intake). More than 95% of cases (NHS Health Check recipients) received a high-quality match, and non-matching participants were dropped from the analysis. A review of the excluded participants indicated that although they tended to be younger, more deprived, and more obese, the main reason for matching failure was the requirement for one-to-one matching within a geographical region. In other words, the matched control for a London health check recipient must also be from London. From this process, we derived a matched sample of 97,204 participants, with 48,602 participants in each exposure group (Fig. 1).
The intervention: NHS Health Check
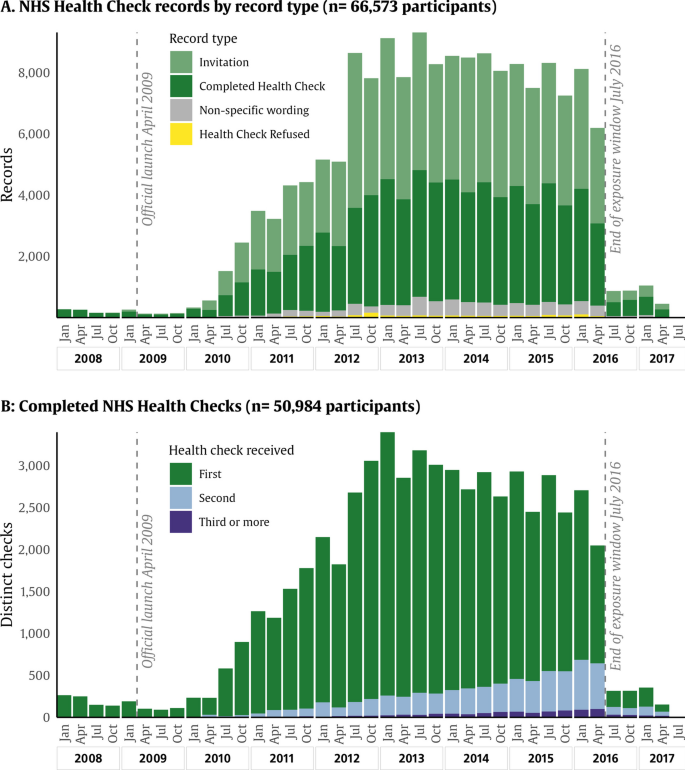
To identify participants who had received an NHS Health Check (or its Scottish equivalent), we performed a text search of primary care clinical records, for the following phrases “keep well, health check, check-up, healthy start, healthy lifestyle, diabetes prevent, well man, well woman, well adult”. This search returned 283,536 records between April 2006 and December 2022. From here, we reviewed the record text to exclude other types of health checks (healthy lifestyle, diabetes management, carer health checks, and unspecified check-ups) and records that did not indicate NHS Health Check completion, for example, invitations (terms including invitation, email, letter), neutral descriptors (not appropriate, indicated, status), and health check refusal (declined, refused, did not attend). The remaining codes that were used to confirm NHS Health Checks are provided in Additional file 1: Table S1. Although the official nationwide launch took place in April 2009, there were some areas that participated in a pilot programme in the year leading up to this date [16]. Within the UK Biobank resource, coverage for primary care records was high up to mid-2016, when the availability of records dropped sharply. Therefore, the exposure window was set between 1 January 2008 and 30 June 2016. The count of records for health check exposure by year is illustrated in Fig. 2. For modelling purposes, we considered the date of exposure to be the date of the first completed NHS Health Check.
NHS Health Check records by year and record type. Distributions describing NHS Health Check records in the UK Biobank. A The distribution of records tagged with NHS Health Check identifiers, coloured by record type, whether the record describes a completed health check, an invitation, a refusal, or a descriptive tag (not necessarily implying completion or refusal). B The distribution of completed health checks, with blue showing the first recorded NHS Health Check and with green and yellow showing follow-up health checks. Participants are included from January 2008 to July 2016
Ascertainment of outcomes
Existing disease at baseline was assessed via both self-report and linked records (hospital and primary care). Incident disease after baseline was ascertained via primary care linked records, hospital records, and death registry (Additional file 1: Table S2), using published code lists where available [17,18,19]. We included the following outcomes: hypertension, diabetes, hyperlipidaemia, stroke (any type), all-cause dementia, myocardial infarction, atrial fibrillation, heart failure, acute kidney injury, chronic kidney disease (stage 3, 4, or 5), fatty liver disease, alcoholic liver disease, liver cirrhosis, liver failure, cardiovascular mortality (death with a primary cause between ICD I00–I80), and all-cause mortality. Participants were followed up until the end of October 2022. All patient consent procedures were completed by the UK Biobank, and details of record linkage in the UK Biobank have been published previously [20].
Definition of covariates
Age, sex, and all other covariates were recorded at baseline. Modelling covariates were selected based on their known associations with outcome risk in previous research; these include age, sex, geographical region, Townsend deprivation score, ethnicity (White/non-White), post-secondary education (yes/no), body mass index, waist-to-hip ratio, current smoking (yes/no), systolic blood pressure, Charlson Comorbidity Index, alcohol intake frequency, physical activity, and fresh vegetable intake. Charlson Comorbidity Index was coded from existing conditions at baseline [21]. Physical activity was coded in summed metabolic equivalent task-minutes per week, based on the aggregation of physical activity fields according to published guidance [22]. To partition participants into geographical regions, we identified the coordinates of six major cities in the mainland UK (London, Bristol, Birmingham, Manchester, Newcastle upon Tyne, and Edinburgh) and then allocated each participant to their nearest city based on the rounded east and north coordinate provided at baseline. Some of the covariates had a small amount of missing values (less than 2%) that were imputed together using multiple imputation with chained equations [23] (summarised in Additional file 1: Table S3).
Statistical analysis
We used graphical illustrations and simple descriptive statistics to outline the features of UK Biobank participants with primary care data and the uptake of the NHS Health Check. To assess the covariate-adjusted differences in outcomes between health check recipients and non-recipients, we used two main modelling approaches.
Time-varying Cox regression
We applied Cox survival modelling with the intervention (NHS Health Check date) coded in a time-varying fashion following the method outlined by Therneau and colleagues [24,25,26]. In this method, follow-up begins at baseline registration, and all participants begin the follow-up period with intervention-negative status, in other words, no NHS Health Check. Then, over time, some participants receive an NHS Health Check, so at that date, they acquire intervention-positive status. Survival models were adjusted by the full complement of covariates outlined above, as recorded at baseline. This analysis makes use of the most amount of data and allows time-based differences in exposure effect to be observed more easily but could still be biased due to residual confounding.
Aligned-start Cox regression
In this analysis, we aligned the intervention window between cases and controls in a manner similar to Sebuødegård and colleagues [27] and then applied proportional hazards regression in the conventional sense. Here, the follow-up period is defined to begin at the date of the completed NHS Health Check, with outcome times aligned accordingly. Each control participant (without an NHS Health Check) is followed up from the intervention date of his or her matched pair. Full follow-up lengths were compared and were not significantly different between the groups. In aligned-start analyses, ages were updated to be consistent with the intervention date, with the remainder of covariates as measured at baseline. This method provides better quality control for known confounding but involves the loss of data, and hence loss in power.
Survival models in both approaches above were adjusted by age, sex, geographical region, Townsend deprivation score, ethnicity, post-secondary education, body mass index, waist-to-hip ratio, current smoking, systolic blood pressure, Charlson Comorbidity Index, alcohol intake frequency, physical activity, and fresh vegetable intake. Aligned-start models were additionally adjusted by the length of time since registration. Multiple testing correction using a false discovery rate of 5% was applied to identify significant p-values across all models.
Further time adjustments
Prior research has identified that NHS Health Check receipt was associated with increased detection and diagnosis of prevalent (but unrecognised) diabetes, hypertension, and cardiovascular and kidney diseases [9]. Therefore, we conducted the survival modelling with three-time exclusion settings: (a) include all outcomes, (b) exclude outcome events in the first 12 months after NHS Health Check, and (c) exclude outcome events in the first 24 months after NHS Health Check. In epidemiological research, it is common to exclude events that occur in the first few years of follow-up when studying the relationship between an exposure and a disease outcome. This latency period intends to reduce bias from reverse causation, which occurs when the main biological processes creating the disease outcome precede the exposure. By removing events that occur in the early years of follow-up, we hope to observe associations between the exposure and disease outcome that are not due to pre-existing disease influencing exposure status (see Rothman and colleagues, p.218–219 [28]), and examples [29, 30]. We tested the proportional hazards assumption for the effect of NHS Health Check on the outcome risk using a chi-square test and graphical display of Schoenfeld residuals. In sensitivity analysis, we re-ran the aligned start Cox models with stratified time periods (Therneau and colleagues [24], Sect. 4). This approach has the lowest power of all, as each coefficient is calculated only using the outcomes within each time stratum.
Unmeasured confounding
Finally, we applied the e-value methodology described by VanderWeele and colleagues [31] to evaluate the potential nullifying impact of unobserved confounding variables. We calculated e-values and their lower bounds for each significant result and provided a translation of these into “years of ageing equivalent” to aid intuitive understanding of their relative strength.
Results
Description of NHS Health Check in the UK Biobank
Within the overall sample (n = 140,899), 66,573 participants (47%) received at least one invitation for an NHS Health Check between January 2008 and June 2016 (Fig. 2). Of those who were invited, 50,984 participants (77% of those invited, 36% of full sample) received an NHS Health Check. Within recipients, most received only one NHS Health Check (44,910, 88%), 10.5% received a second NHS Health Check, and 1.4% received three or more.
In the full sample, there were more women than men (59% compared to 41%), with participants fairly evenly spread across the age range from 40 to 70 years at baseline (Fig. 3). Eighteen per cent of participants were obese (with body mass index > 30 kg/m2), and 10.6% were current smokers. Overall, 29.3% of participants had a Townsend deprivation index above the 2011 UK median indicating lower-than-average deprivation in the study sample [32]. This varied by geographical region, with London participants having the most nationally representative deprivation with 52.3% of participants above the UK median. NHS Health Check uptake rates also varied by geographical region, with the highest uptake in Birmingham, Manchester, and Newcastle regions (all above 40%), with the lowest uptake observed in Scotland (8.2%).
Summary of NHS Health Check in UK Biobank participants. A Overall summaries for the sample of UK Biobank participants with primary care available (n = 140,772). B Summary of geographical locations. C Sample characteristics by geographical region. Deprivation proportion refers to the proportion of the sample that fall above the UK median for socio-economic deprivation according to reported Townsend deprivation scores and quintiles from the 2011 census
The matched modelling set and observed outcomes
The matched subset used for modelling was very similar in profile to the overall study set, with 95% of NHS Health Check recipients (48,602/50,984) receiving a high-quality matched control pair (Table 1).
Characteristic of the UK Biobank more generally, the sample was mostly White ethnicity (4% other ethnicities), mostly physically active (23% inactive), with 19% of the sample consuming alcohol at least once per day. Table 1 also reports the outcome counts observed in the matched groups, along with their percentage rates. Many of the reported outcome rates are similar between the groups (hypertension, diabetes, stroke, heart failure, chronic kidney disease). For several outcomes, there are larger differences between cases and controls, for example, all-cause dementia (1.2% vs 1.4%), myocardial infarction (1.9% vs 2.2%), and acute kidney injury (4.0% vs 5.3%). In Fig. 4, histogram plots of outcome counts in NHS Health Check recipients are overlaid with the time-aligned outcome counts observed in their matched counterparts. Interestingly, for some outcomes (hypertension, diabetes, high cholesterol, chronic kidney disease, fatty liver disease and liver failure), more new diagnoses were recorded in NHS Health Check recipients in the initial 2-year period following the health check than in their matched pairs. On the other hand, following the 2-year mark, outcome counts were more likely to be equal or slightly higher in people who did not receive the NHS Health Check.
Outcomes during follow-up in NHS Health Check recipients and their matched controls. Bars show the counts of participants receiving condition diagnoses for the first time, in the years following the NHS Health Check in health check recipients and in the aligned exposure window in the covariate-matched control cohort. The dark teal shows the counts where both groups are equal, the bright purple indicates where the health check group counts are greater, and the bright green indicates where control counts are greater. The 2-year initial period following the health check is marked with a black vertical line
NHS Health Check associations with outcomes
Because the smoothed Schoenfeld residual curves and chi-square tests indicated departures from proportionality for several of the outcomes studied (Additional file 1: Fig. S1), we applied time stratification and two types of time-dependent modelling. In time-varying survival models, the time effect is demonstrated clearly. For some outcomes, the fully adjusted diagnosis rate was significantly higher in NHS Health Check recipients (Fig. 5 and Additional file 1: Table S4). When early events (in the first 12 months) were included, diagnoses of hypertension were 6% higher in the NHS Health Check group, with additional higher rates for high cholesterol (11%), chronic kidney disease (15%), and fatty liver disease (17%). However, when the initial 12 or 24 months were excluded from the model, the overall hazards across all outcomes were significantly lower in NHS Health Check recipients, with average risk reductions between 20 and 40% (hazard ratios between 0.6 and 0.8).
Associations between NHS Health Check and incident outcomes. Points represent hazard ratios, and horizontal bars represent 95% confidence intervals for hazard ratios from Cox proportional hazards models associating completed NHS Health Check with new diagnoses received during follow-up. A Hazard ratios from models with time-varying exposure. B Hazard ratios from models with aligned follow-up start times. The results shown in faded/greyed out colour were not significant after applying multiple testing correction with a 5% false discovery rate. Colours indicate that models were computed with three outcome exclusion settings (green (0) = including all outcomes, aqua blue (12) = excluding outcomes in the first 12 months after NHS Health Check, navy blue (24) = excluding outcomes in the first 24 months after NHS Health Check). Models are adjusted by age, sex, geographical region, Townsend deprivation score, ethnicity, body mass index, waist-hip ratio, smoking, systolic blood pressure, alcohol intake frequency, physical activity, daily vegetable/salad intake, and Charlson Comorbidity Index
In aligned-start regression models, early-event time effects are much less pronounced (Fig. 5 and Additional file 1: Table S4). In these fully adjusted models, NHS Health Check recipients had significantly lower diagnosis rates for all-cause dementia (19% lower, hazard ratio (HR) 0.81), myocardial infarction (15% lower, HR 0.85), atrial fibrillation (9% lower, HR 0.91), acute kidney injury (23% lower, HR 0.77), liver cirrhosis (44% lower, HR 0.66), and all-cause mortality and cardiovascular mortality (both 23% lower, with HR 0.77).
The significant early effects observed in the main analysis were confirmed in sensitivity analysis by applying time stratification to the aligned-start models (Additional file 1: Fig. S2), with the addition of significantly higher rates of diabetes diagnosed in the first year of follow-up. Time-stratified models characterised significantly reduced longer-term risk for the same disease outcomes identified in the main aligned-start models.
Application of e-values to the regression results (Additional file 1: Table S5) found moderate robustness of most observed hazard ratios to unmeasured confounding. The results for acute kidney injury, liver cirrhosis, and myocardial infarction had stronger e-values (less likely to be rendered insignificant by unmeasured confounders), while the e-values for all-cause dementia and atrial fibrillation were weak, meaning that even quite a weak unmeasured confounding variable could render our result non-significant.
Discussion
In this large community-based sample from the UK Biobank across an average of 9 years of prospective follow-up, receipt of the NHS Health Check was related to reduced long-term risk of all-cause and cardiovascular disease mortality and reduced incidence of disease across the liver, kidney, heart, and brain organ systems. In analyses including the early follow-up period, those who had the NHS Health check had increased detection of hypertension, high cholesterol, and chronic kidney disease. This effect was not observed in analyses restricting follow-up to beyond 24 months after the Health Check, indicating that these increased diagnoses indicate heightened detection of undiagnosed or quiescent pre-clinical disease, the treatment of which likely contributes to the reduction in health outcomes observed in the longer term.
The existing evidence on the effect of the NHS Health Check programme so far is mixed [9]. Some studies have found that the programme is associated with small reductions in the risk of cardiovascular disease and diabetes, while others have found no significant benefit. In a 5-year study of electronic health records from several London commissioning groups, Robson et al. found that NHS Health Check attendees had a higher short-term likelihood of a diagnosis of type 2 diabetes, hypertension, and chronic kidney disease and receive treatment with statins and antihypertensives [33]. These findings were subsequently confirmed in a large nationally representative sample (QDatabase) [34].
Using a similar approach to the current work, Chang and colleagues [35] used a matched sample from the Clinical Practice Research Datalink (CPRD, with n = 29,672 in each group) to find evidence of an overall reduction in cardiovascular risk as computed by QRISK2 in NHS Health Check participants, and a significant increase in diagnoses for hypertension and diabetes. This study was unable to detect differences in longer-term outcomes with a median follow-up time of 2 years.
Our findings corroborate these observations in a much larger independent cohort by demonstrating an increased diagnosis of incident hypertension, high cholesterol, and chronic kidney disease in the immediate period after the NHS Health Check. These conditions are typically asymptomatic with a long pre-clinical phase. As such, they are almost always identified through screening or opportunistic diagnosis. The longer follow-up duration in our study enabled us to extend existing knowledge by demonstrating that this apparent increase in diagnosis is confined to the first 2 years after the NHS Health Check, after which the risk of incident health events is significantly lower in recipients.
Our study is the first to demonstrate an association between receipt of the NHS Health Check and reduction in long-term risk of multiorgan outcomes. We do not assert that significant changes flow directly from a single 15-min appointment. It is more plausible that longer-term trajectory changes arise from (1) increased detection and treatment of risk factors (such as diabetes, hypertension, and high cholesterol), (2) more regular face-to-face reinforcement towards healthy behaviour change (like exercise and smoking cessation), and (3) better management of underlying active disease processes like atherosclerosis and atrial fibrillation. These processes work together to reduce the risk of long-term illnesses in NHS Health Check recipients. The initial health check visit sets up a relationship with the primary healthcare team, which may not otherwise occur in ostensibly healthy people. Although a recent review has found wide variation in practice [12], the health check system is specifically designed to facilitate access to further healthcare services, increasing subsequent healthcare utilisation and providing further opportunities for appropriate screening and risk factor optimisation.
The uptake of the NHS Health Check is an active area of research. Several recent studies [36, 37] have identified a range of factors influencing health check uptake. In 2018/2019, Public Health England published an uptake rate for England at 45.9% of those invited [9]. This figure is corroborated by a study of primary care records in England over a similar time period as our study, which reports an uptake rate of 52.6% of those invited [38]. The overall health check rate of 36.2% observed in this study is in line with an invitation rate of 80% of those eligible and an uptake rate of 45%.
Some studies have also found that NHS Health Check is associated with improvements in health behaviours such as smoking cessation, physical activity, and diet and with better management of hypertension and hypercholesterolaemia [11, 39]. But also, it has been found that the programme has not reached everyone who would benefit, particularly those in more deprived areas, and that the programme’s effectiveness may have been limited by a lack of follow-up and support for lifestyle changes [9]. Using a health economics modelling approach, Thomas and colleagues [40] did not report differences in the outcomes but still found that NHS Health Check would generate significant cost savings from improved detection of cardiovascular risk factors such as diabetes and high cholesterol.
Limitations
We recognise that the UK Biobank cohort is known to be healthier on average than the general UK population [41, 42], meaning that the rates of incident disease observed in the current study are likely to be lower than the UK average incidence rates [43]. Similarly, while this study found significant differences in the outcome rates overall, the exact size of any effects would need to be validated in a nationally representative cohort.
In addition, self-selection bias is a very important factor to consider when assessing the effectiveness of any voluntary intervention like the NHS Health Check. People who engage with health screening programmes are systematically different in important ways from those who do not. They tend to have a more favourable social, lifestyle, and health profile compared to non-attenders. Studies evaluating the clinical value of screening programmes for the prevention of health outcomes are highly susceptible to confounding by these factors, which can be challenging to capture and include in modelling adjustments [34]. In our study, we created a comparator cohort of health check non-attenders matched to recipients on an extensive range of social, demographic, and clinical factors, with descriptive analyses confirming high-quality matching on variables considered. These findings suggest that the observed associations in our study may be inflated, but not fully explained, by self-selection bias in the NHS Health Check recipient group.
The UK Biobank is subject to participation bias [44]. The extensive measurements taken at baseline recruitment are likely to have made all participants more aware of their cardiovascular risk and in turn influenced their decision to independently take part in the NHS Health Check programme. For the purposes of this study, however, all participants (both cases and controls) would be subject to this bias equally.
Finding evidence linking any intervention with longer-term outcomes can be challenging, due to the differences in implementation times and the abundance of potentially confounding factors. Although we have adjusted for a number of important confounders, there could still be residual uncaptured confounding associated with UK Biobank membership and attendance at NHS Health Checks. While we have explored several regression methods, future work could study a larger matched cohort of participants receiving their first NHS Health Check at the same time, to remove potential confounding associated with time differences. Lastly, the intervention and outcome variables in this study are both defined via electronic health records; therefore, the accuracy of both measures is limited by the quality and timeliness of the data coding and the integrity of data linkage [45].
Conclusions
This study demonstrates that proactive, well-designed preventive programmes such as the NHS Health Check can be effective in reducing longer-term disease outcomes, across multiple organ systems. Overall, our results suggest that the NHS Health Check has a role in preventing long-term diseases through risk factor modification and that this effect is independent of any risk-modifying behaviours the participants may pursue otherwise. While it remains challenging to gather evidence-based data to evaluate screening programmes, our work goes some way in addressing methodological issues that have hampered previous studies and provide further evidence in support of the NHS Health Check as a preventive public health programme. This research is an important addition to a growing body of work supporting the long-term benefits of a programme such as NHS Health Check and its effectiveness for potential multimorbidity prevention.
Availability of data and materials
This research was conducted using the UK Biobank resource under access application 59,867. The UK Biobank will make the data available to all bona fide researchers for all types of health-related research that is in the public interest, without preferential or exclusive access for any persons. All researchers will be subject to the same application process and approval criteria as specified by the UK Biobank. For more details on the access procedure, see the UK Biobank website: https://www.ukbiobank.ac.uk/enable-your-research/register.
Abbreviations
- UK:
-
United Kingdom
- NHS:
-
National Health Service
- ICD:
-
International Classification of Diseases
- HR:
-
Hazard ratio
References
Marthias T, Anindya K, Ng N, McPake B, Atun R, Arfyanto H, et al. Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open. 2021;11(2):e041870.
Head A, Fleming K, Kypridemos C, Pearson-Stuttard J, O’Flaherty M. Multimorbidity: the case for prevention. J Epidemiol Commun Health. 2021;75(3):242–4.
NHS. The NHS Long Term Plan. 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf. Accessed 02 Nov 2023.
Matthews J. We need a shift from reactive to proactive care. BMJ. 2012;344:e1225.
Hylton K, Thompson K, Kearney M, Lagord C. NHS Health Check Best practice guidance: for commissioners and providers (Public Health England). 2019. https://www.healthcheck.nhs.uk/commissioners-and-providers/national-guidance/. Accessed 02 Nov 2023.
Dalton ARH, Bottle A, Okoro C, Majeed A, Millett C. Implementation of the NHS health checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting. Fam Pract. 2011;28(1):34–40.
Muirie J, McCartney G, Fischbacher C, Lewsey J, Connolly J. The impact of Keep Well: an evaluation of the Keep Well Programme from 2006 to 2012 (NHS Health Scotland). 2014. https://www.healthscotland.scot/publications/keep-well-national-programme. Accessed 28 Sep 2023.
Public Health Scotland. Keep Well. 2020. https://www.healthscotland.com/keep-well.aspx. Accessed 21 Sep 2023.
Tanner L, Kenny R, Still M, Ling J, Pearson F, Thompson K, et al. NHS health check programme: a rapid review update. BMJ Open. 2022;12(2):e052832.
Usher-Smith JA, Harte E, MacLure C, Martin A, Saunders CL, Meads C, et al. Patient experience of NHS health checks: a systematic review and qualitative synthesis. BMJ Open. 2017;7(8):e017169.
Debiec R, Lawday D, Bountziouka V, Beeston E, Greengrass C, Bramley R, et al. Evaluating the clinical effectiveness of the NHS health check programme: a prospective analysis in the Genetics and Vascular health check (GENVASC) study. BMJ Open. 2023;13(5):e068025.
Duddy C, Gadsby E, Hibberd V, Krska J, Wong G. Understanding what happens to attendees after an NHS health check: a realist review. BMJ Open. 2022;12(11):e064237.
Jain R, Stone JA, Agarwal G, Andrade JG, Bacon SL, Bajaj HS, et al. Canadian cardiovascular harmonized National Guideline Endeavour (C-CHANGE) guideline for the prevention and management of cardiovascular disease in primary care: 2022 update. CMAJ. 2022;194(43):e1460–80.
Fegers-Wustrow I, Gianos E, Halle M, Yang E. Comparison of American and European guidelines for primary prevention of cardiovascular disease: JACC guideline comparison. J Am Coll Cardiol. 2022;79(13):1304–13.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–61.
Perry C, Thurston M, Alford S, Cushing J, Panter L. The NHS health check programme in England: a qualitative study. Health Promot Int. 2016;31(1):106–15.
UK Biobank. Code lists for health outcomes. 2020. https://biobank.ndph.ox.ac.uk/showcase/refer.cgi?id=594. Accessed 23 Mar 2022
Hagström H, Adams LA, Allen AM, Byrne CD, Chang Y, Grønbæk H, et al. Administrative coding in electronic health care record-based research of NAFLD: an expert panel consensus statement. Hepatology. 2021;74(1):474–82.
Dolezalova N, Reed AB, Despotovic A, Obika BD, Morelli D, Aral M, et al. Development of an accessible 10-year digital CArdioVAscular (DiCAVA) risk assessment: a UK Biobank study. Eur Heart J- Digital Health. 2021;2(3):528–38.
Caleyachetty R, Littlejohns T, Lacey B, Bešević J, Conroy M, Collins R, et al. United Kingdom biobank (UK Biobank): JACC focus seminar 6/8. J Am Coll Cardiol. 2021;78(1):56–65.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
The IPAQ group. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ ) – short and long forms. 2005. https://biobank.ndph.ox.ac.uk/ukb/ukb/docs/ipaq_analysis.pdf. Accessed 21 Oct 2021.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67.
Therneau T, Crowson C, Atkinson E. Using time dependent covariates and time dependent coefficients in the Cox model. Survival Vignettes. 2017;2(3):1–25.
Zhang Z, Reinikainen J, Adeleke KA, Pieterse ME, Groothuis-Oudshoorn CGM. Time-varying covariates and coefficients in Cox regression models. Ann Transl Med. 2018;6(7):121.
Shintani AK, Girard TD, Eden SK, Arbogast PG, Moons KGM, Ely EW. Immortal time bias in critical care research: application of time-varying Cox regression for observational cohort studies. Crit Care Med. 2009;37(11):2939–45.
Sebuødegård S, Botteri E, Hofvind S. Breast cancer mortality after implementation of organized population-based breast cancer screening in Norway. JNCI: J Natl Cancer Institute. 2020;112(8):839–46.
Rothman KJ, Lash TL. Modern epidemiology. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2015.
Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Meir S, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996;313(7049):84–90.
Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380(9852):1491–7.
Van Der Weele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74.
UK Data Service. 2011 UK Townsend Deprivation Scores. 2021. https://statistics.ukdataservice.ac.uk/dataset/2011-uk-townsend-deprivation-scores. Accessed 13 Feb 2023
Robson J, Dostal I, Madurasinghe V, Sheikh A, Hull S, Boomla K, et al. NHS health check comorbidity and management: an observational matched study in primary care. Br J Gen Pract. 2017;67(655):e86-93.
Robson J, Garriga C, Coupland C, Hippisley-Cox J. NHS health checks: an observational study of equity and outcomes 2009–2017. Br J Gen Pract. 2021;71(710):e701–10.
Chang KCM, Lee JT, Vamos EP, Soljak M, Johnston D, Khunti K, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ. 2016;188(10):e228–38.
Cook EJ, Sharp C, Randhawa G, Guppy A, Gangotra R, Cox J. Who uses NHS health checks? Investigating the impact of ethnicity and gender and method of invitation on uptake of NHS health checks. Int J Equity Health. 2016;15(1):13.
Bunten A, Porter L, Gold N, Bogle V. A systematic review of factors influencing NHS health check uptake: invitation methods, patient characteristics, and the impact of interventions. BMC Public Health. 2020;20(1):93.
Patel R, Barnard S, Thompson K, Lagord C, Clegg E, Worrall R, et al. Evaluation of the uptake and delivery of the NHS Health Check programme in England, using primary care data from 9.5 million people: a cross-sectional study. BMJ Open. 2020;10(11):e042963.
Alageel S, Gulliford MC. Health checks and cardiovascular risk factor values over six years’ follow-up: matched cohort study using electronic health records in England. Sheikh A, editor. PLoS Med. 2019;16(7):e1002863.
Thomas C, Brennan A, Goka E, Squires HY, Brenner G, Bagguley D, et al. What are the cost-savings and health benefits of improving detection and management for six high cardiovascular risk conditions in England? An economic evaluation. BMJ Open. 2020;10(9):e037486.
Keyes KM, Westreich D. UK Biobank, big data, and the consequences of non-representativeness. Lancet. 2019;393(10178):1297.
Swanson JM, The UK. Biobank and selection bias. Lancet. 2012;380(9837):110.
Public Health England. Briefing document: first incidence of stroke—estimates for England 2007 to 2016. 2018. https://www.gov.uk/government/publications/first-stroke-estimates-in-england-2007-to-2016. Accessed 02 Nov 2023
Schoeler T, Speed D, Porcu E, Pirastu N, Pingault JB, Kutalik Z. Participation bias in the UK Biobank distorts genetic associations and downstream analyses. Nat Hum Behav. 2023;7(7):1216–27.
Adamska L, Allen N, Flaig R, Sudlow C, Lay M, Landray M. Challenges of linking to routine healthcare records in UK Biobank. Trials. 2015;16(2):O68.
Acknowledgements
Not applicable.
Funding
SN, BR, and CM were supported by the Oxford NIHR Biomedical Research Centre (IS-BRC-1215–20008), the Oxford British Heart Foundation Centre of Research Excellence. LS received funding from the European Association of Cardiovascular Imaging (EACVI Research Grant App000076437) and the Barts Charity (G-002389). ZRE recognises the National Institute for Health Research (NIHR) Integrated Academic Training programme which supports her Academic Clinical Lectureship post and was also supported by the British Heart Foundation Clinical Research Training Fellowship No. FS/17/81/33318. SEP acknowledges support from the “SmartHeart” EPSRC programme grant (www. nihr.ac.uk; EP/P001009/1). SEP has also received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 825903 (euCanSHare project). AT is supported by a Wellcome Trust (https://wellcome.org/) fellowship (216462/Z/19/Z). MH is supported by the Wellcome Trust (206330/Z/17/Z) and NIHR Oxford Biomedical Research Centre (IS-BRC-1215–20008). TEN is supported by the Li Ka Shing Centre for Health Information and Discovery, an NIH grant (https://www.nih.gov/, TN: R01EB026859); the NIHR Oxford Biomedical Research Centre (BRC-1215–20014); and a Wellcome Trust award (TN: 100309/Z/12/Z). This work includes data provided by patients and collected by the NHS and NHS Digital as part of their care and support. The research was supported by the Wellcome Trust Core Award Grant Number 203141/Z/16/Z with funding from the NIHR Oxford BRC. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. This research used data assets made available by the National Safe Haven as part of the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation (MCPC20058).
Author information
Authors and Affiliations
Contributions
The study was conceived by TEN, SN, SEP, and CM. CM and TEN formulated the statistical analysis plan. CM led and performed the analysis and led the writing of the manuscript. ZRE and LS contributed to the drafting of the manuscript. All co-authors including JR, BR, AT, AR-F, and MH provided critical review of the work. All authors read and approved the final manuscript. TEN and SN provided overall supervision for the work. TEN and SN are the guarantors of the work. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Authors’ Twitter handles
@CelMcC (Celeste McCracken); @BR_CMR (Betty Raman); @AnyaTopiwala (Anya Topiwala); @MasudHusain (Masud Husain).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study complies with the Declaration of Helsinki; the work was covered by the ethical approval for UK Biobank studies from the National Health Service (NHS) National Research Ethics Service on 17 June 2011 (Ref 11/NW/0382) and extended on 18 June 2021 (Ref 21/NW/0157) with written informed consent obtained from all participants. This study was conducted under UK Biobank access application 59867.
Consent for publication
This study contains no identifying information for any person or persons. All UK Biobank have given consent for their data to be published as part of the general consent for UK Biobank registration.
Competing interests
SEP provides consultancy to Cardiovascular Imaging Inc., Calgary, Alberta, Canada. BR consulted for Axcella Therapeutics. ARF is an employee and shareholder in Perspectum Ltd., Oxford, UK. SN is a founder, shareholder, and former board member of Perspectum. TEN provides consultancy to Perspectum Ltd., Oxford, UK. All other authors declare that they have no competing interests. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Checklist S1.
STROBE Checklist. Table S1. UK Biobank-specific primary care codes used to identify NHS Health Check exposure. Table S2. UK Biobank fields and codes for ascertainment of outcomes. Table S3. Missing value imputation details for sample covariates. Fig. S1. Visualisation of the time-varying hazard effects. Table S4. Hazard ratios, 95% confidence intervals and p-values for associations between NHS Health Check and incident diagnoses. Fig. S2. Sensitivity analysis with stratified time periods. Table S5. E-value lower bounds for significant hazard ratios.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McCracken, C., Raisi-Estabragh, Z., Szabo, L. et al. NHS Health Check attendance is associated with reduced multiorgan disease risk: a matched cohort study in the UK Biobank. BMC Med 22, 1 (2024). https://doi.org/10.1186/s12916-023-03187-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-03187-w