- Research article
- Open access
- Published:
Association of breastfeeding with mental disorders in mother and child: a systematic review and meta-analysis
BMC Medicine volume 21, Article number: 393 (2023)
Abstract
Background
Breastfeeding has long been associated with numerous benefits for both mothers and infants. While some observational studies have explored the relationship between breastfeeding and mental health outcomes in mothers and children, a systematic review of the available evidence is lacking. The purpose of this study is to systematically evaluate the association between breastfeeding and mental health disorders in mothers and children.
Methods
We systematically searched MEDLINE and EMBASE from inception to June 2, 2023. The inclusion criteria consisted of all studies evaluating links between breastfeeding and development of mental health disorders in children and mothers. Risk of bias was assessed using the Newcastle–Ottawa Scale (NOS) while grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the certainty of evidence. A random-effects meta-analysis was used if possible, to estimate the odds ratio for the association between breastfeeding and mental health outcomes. The Mantel–Haenszel method was utilised for pooling ORs across studies. Study heterogeneity was assessed using the I2 statistic.
Results
Our review identified twenty-one original study. Of these, 18 focused on the association between breastfeeding and child health, assessing depressive disorders, schizophrenia, anxiety disorders, eating disorders and borderline personality disorder. Three studies evaluated the associations between breastfeeding and maternal mental health disorders. Three studies looking at outcomes in children showed no significant association between breastfeeding and occurrence of schizophrenia later in life (OR 0.98; 95% CI 0.57–1.71; I2 = 29%). For depressive disorders (5 studies) and anxiety disorders (3 studies), we found conflicting evidence with some studies showing a small protective effect while others found no effect. The GRADE certainty for all these findings was very low due to multiple limitations. Three studies looking at association between breastfeeding and maternal mental health, were too heterogeneous to draw any firm conclusions.
Conclusions
We found limited evidence to support a protective association between breastfeeding and the development of mental health disorders in children later in life. The data regarding the association between breastfeeding and maternal mental health beyond the postnatal period is also limited. The methodological limitations of the published literature prevent definitive conclusions, and further research is needed to better understand the relationship between breastfeeding and mental health in mothers and children.
Introduction
Mental health disorders continue to be a major global medical and societal burden, affecting individuals of all ages. These disorders are linked to significant morbidity, disability, and mortality rates [1, 2]. Prior to the COVID-19 pandemic, the Global Burden of Disease Study estimated that 264 million people worldwide suffered from depression, while bipolar disorder and schizophrenia affected 45 million and 20 million individuals respectively [3]. The COVID-19 pandemic additionally resulted in increase in prevalence of major depressive disorder and anxiety disorders [4]. Individuals residing in regions with political, social, and humanitarian problems are particularly susceptible to mental health disorders [2]. In developed countries, patients often face stigmatisation and neglect by society [2, 5, 6].
The aetiology and mechanisms of mental disorders are complex and not fully understood with multiple factors, hereditary, social and environmental, proposed among the main contributors to their development which limits potential for preventive measures [7]. Potential exposures during infancy and early childhood were extensively investigated and associations with mental health disorders development were reported [8].
Breastfeeding is associated with multiple beneficial effects for maternal and child health. Leading local and international organisations, such as the World Health Organization (WHO) [9], the European Commission for Public Health (ECPH) [10] and the American Academy of Pediatrics (AAP), produced guidelines recognising exclusive breastfeeding as an optimal feeding method during the first 6 months of life [11]. Breastfeeding is a well-established contributor both to child socioemotional and neurocognitive development [12, 13]. The reason commonly named behind this association is presence of potentially beneficial constituents, such as immunological biomarkers and long-chain polyunsaturated fatty acids (LC-PUFAs), that cannot be fully replaced by human milk substitutes [14,15,16], association between breastfeeding and attachment [17], skin-to-skin contact and socio-emotional aspects [14].
Although some attempts to investigate associations between breastfeeding and mental disorders were made, comprehensive assessment of available evidence is still lacking. Therefore, the aim of this systematic review is to comprehensively assess available up to date evidence on the associations between breastfeeding and development of mental health disorders in children and mothers to provide an impetus for further research in the field and improve our understanding of the topic.
Methods
This systematic review is reported in accordance with the recommendations set forth by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18]. The review protocol was registered with the National Institute for Health Research’s PROSPERO a priori (PROSPERO 2019 CRD42019134214).
Search and screening
Studies were identified through searches of two electronic databases (Medline and Embase via OVID) from inception to June 3, 2021, using both free text and medical subject headings (MeSH) terms. Additional search was performed on June 2, 2023, to screen for recent papers. The search strategies are presented in Additional file 1: Box S1. In addition, the publications cited in the reference lists of the included studies and previously published review articles were carefully screened to ensure that no original published data had been missed.
Pairs of authors (PB, IA, DB, AM and RB) independently conducted the title and abstract screening. Any disagreements between the screeners were resolved via consensus or a third reviewer (DM).
Eligibility criteria
Types of studies
Any randomised controlled trials (RCTs), quasi-RCTs, as well as cohort (prospective or retrospective) studies, nested case–control studies, other case–control studies and cross-sectional studies (including those with retrospective data) were included.
Types of participants
No restrictions to specific population and high-risk groups (e.g. cohorts of patients with family history of mental illnesses) were applied.
Types of interventions or exposures
Type/duration of breastfeeding. Our systematic review encompassed all infants who were fed breast milk, irrespective of whether it was delivered directly through breastfeeding or administered via a bottle of expressed milk.
Comparator
The comparison was made with the individuals who were not breastfed (any other type of feeding) and/or breastfeeding of varying duration.
Outcomes of interest
The outcomes of interest are as follows: depressive disorders, bipolar disorder, anxiety disorders, phobia, social anxiety disorders, panic disorder, obsessive–compulsive disorder, separation anxiety disorder, personality disorders, neuroticism, feeding and eating disorders, anorexia, bulimia, binge eating disorder, posttraumatic stress disorder, dysphoria, dissociative disorders, schizophrenia, anaclitic depression, attachment, suicide, alcohol addiction. We did not apply any restrictions pertaining to the diagnosis of the condition.
This systematic review delved into the associations between breastfeeding and designated mental health outcomes, separately assessing these relationships for (a) children and (b) mothers.
Studies with follow-up period less than 12 months since birth were excluded. Manuscripts investigating associations between breastfeeding and autism spectrum disorders (ASD) and attention deficit hyperactivity disorders (ADHD) were excluded, as systematic reviews regarding these conditions were published recently [19, 20]. Premature infants are at an increased risk for chronic medical conditions and developmental outcomes, including mental health disorders [21]. However, the underlying factors that contribute to these risks may differ from those in full-term infants. Therefore, including studies that focus specifically on premature infants may introduce heterogeneity into the analysis, making it difficult to draw conclusions about the association between breastfeeding and mental health outcomes in a general population. To ensure the validity and generalisability of the results, we excluded research papers in which the subjects were premature infants from this systematic review. We also excluded studies providing no specific diagnosis in patients within the cohort of interest. As this topic has been addressed in a previous systematic review, studies examining the relationship between breastfeeding and postnatal maternal depression were excluded [22].
Data extraction
Pairs of authors (PB, IA, DB, AM, AP and RB) independently conducted the data extraction. The extracted data included study design, country of the study, population characteristics, age of children or/and follow-up period, sample size and follow-up rate, number of cases and controls in exposed and non-exposed group, definition of exposure and outcome, methods of outcome assessment, effect estimates with 95% Cis and confounders included in the analysis.
Data synthesis
All studies included in the systematic review were grouped by the outcome of interest and study type and then further grouped according to the type and/or duration of breastfeeding and effect measure (e.g. odds ratio, hazard ratio). Final groups with three or more studies with comparable exposure and outcome definition were considered suitable for meta-analysis. For outcomes where the original studies did not report both the number of participants in the exposed and non-exposed groups and the odds ratios, meta-analysis was not conducted. This is because such information is necessary to calculate the weights of the studies and estimate the overall effect size.
A random-effects meta-analysis was conducted to estimate the odds ratio (OR) and corresponding 95% confidence interval for the association between breastfeeding and mental health outcomes. The Mantel–Haenszel method was used to pool the Ors across studies. The results were considered statistically significant if the 95% CI did not include the null value of 1.0. Heterogeneity across studies was assessed using the I-squared (I2) statistic.
Risk of bias assessment
Risk of bias assessment was performed by two authors (PB and RB or YET) independently using Newcastle–Ottawa Scale (NOS), which provides different assessment strategies for case–control and cohort studies [23]. Assessment according to NOS total score was reported as follows: very good = 9–10, good = 7–8, satisfactory = 5–6, unsatisfactory = 0–4. Selection of NOS instead of Risk Of Bias In Non-randomised Studies—of Interventions (ROBINS-I) was based on similar reliability but better applicability [24]. Results of NOS evaluation are outlined in Additional file 1: Tables S1–S3.
The grading of Recommendations, Assessment and Evaluation (GRADE) approach was used to evaluate the certainty of evidence for diseases of interest where pooled analyses and/or narrative synthesis was possible. As per suggested approach it was classified into high, moderate, low and very low [25]. Data from observational studies were considered low-quality evidence unless there was plausible evidence which would suggest upgrade of evidence certainty [26].
Results
Synthesis
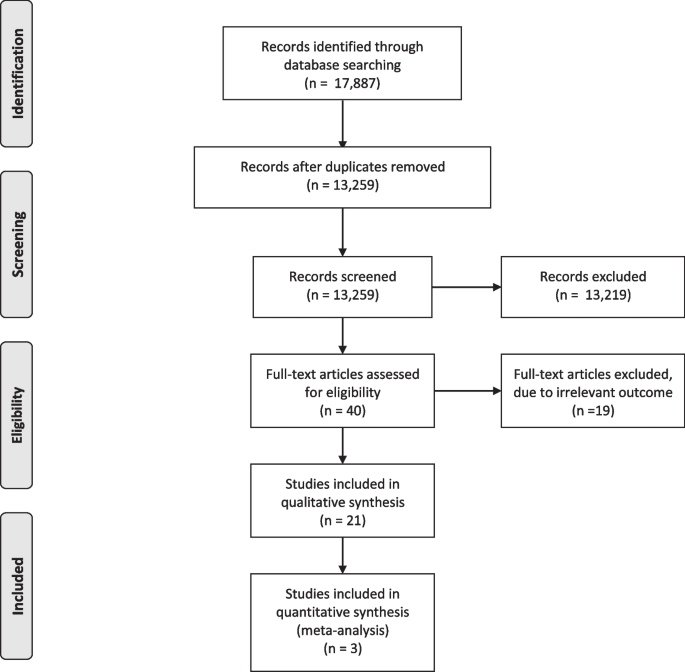
A total of 17,887 items were identified through initial searches, and 40 articles met the inclusion criteria after duplicate removal and title/abstract screening (Fig. 1). Full-text manuscripts were assessed, and 19 articles were excluded, resulting in 21 articles included in the qualitative synthesis, with 18 investigating association between breastfeeding and child health and three looking at maternal health outcomes. Of these, three studies were included in the quantitative synthesis for the outcome of schizophrenia. The included studies were published between 1997 and 2023 and were all observational, comprising of 6 case–control studies [27,28,29,30,31,32], 5 retrospective studies [33,34,35,36,37] and 9 prospective cohort studies [38,39,40,41,42,43,44,45,46] and one cross-sectional study with retrospective assessment of the exposure [47].
The studies investigated associations between breastfeeding and mental health disorders in children and maternal mental health disorders. Specifically, eight studies assessed depressive disorders [33, 34, 36, 40, 41, 43, 45, 47], six investigated schizophrenia [28,29,30, 32, 37, 38] and five looked at anxiety disorders [31, 41, 43, 45, 47], while eating disorders [42] and borderline personality disorder [27] were assessed in one study each. In one study, the prevalence of mental health disorders in children was described without specifying the outcome [44].
Three studies evaluated the associations between breastfeeding and maternal mental health disorders [35, 39, 46].
Participant characteristics
Studies were carried out in twelve different countries, with the majority of the research being conducted in the European and Australasian regions. There were three studies conducted in China [33, 34, 40], three in the USA [36, 39, 42], three in Australia [41, 43, 46], and in the United Kingdom [32, 37, 47], two in Brazil [44, 45] and one each in South Korea [35], Japan [29], South Africa[28], Italy [30], Turkey [31], Denmark [38] and Germany [27].
Sample size ranged from 160 [39] to 186,452 [25] participants in cohort studies and between 100 [28] and 450 [31] in case–control studies. Most of the studies followed children up to the adolescence with the maximum follow-up duration of 40 years.
Breastfeeding definition and reporting
There was a substantial variation in breastfeeding reporting and definitions used. Some studies collected already predefined data from the registries [46], others used structured standardised (e.g. Pre-/Postnatal Stress Questionnaire (NPQ-PSQ) [27], Growing Up Today Study (GUTS) questionnaire [42]) and non-standardised questionnaires and interviews [28, 30, 41, 44, 45, 47, 31,32,33,34, 36, 37, 39, 40] obtaining the data prospectively or retrospectively. Exclusive breastfeeding was usually defined as breastfeeding without intake of “any other food”.
Association between breastfeeding and mental health in children
Schizophrenia
Six studies investigated schizophrenia, with four using case–control design [28,29,30, 32], and two cohort studies, a prospective [38] and a retrospective [37] (Table 1). The outcome of interest was defined in accordance with Diagnostic and Statistical Manual of Mental Disorders (DSM)-III [32], DSM-IV [28,29,30], ICD 9 [37], International Classification of Diseases (ICD)-8 code 295 or ICD-10 code F20 [28]. In a single study, Sorensen and co-authors defined schizophrenia as bizarre delusions, delusions of control, abnormal affect, autism, hallucinations and disorganised thinking [38].
The study risk of bias determined by means of NOS was good in cohort studies, while case–control studies were generally of satisfactory risk of bias (range satisfactory to good). The common flaw was lack of adjustment for potentially significant confounders such as family history of schizophrenia, with four studies presenting crude data only [28,29,30, 37]. Exposure to breastfeeding was self-reported by parents, and for several case–control studies, the recall period exceeded 20 years [32, 37, 38].
All but one study [38] found no association between breastfeeding and schizophrenia, Sorensen et al. reported an association between breastfeeding for two weeks or less and increased risk of schizophrenia adjOR 1.73 (95% CI 1.13–2.67) upon adjustment for maternal schizophrenia, single mother status, sex and parental social status at 1 year of age.
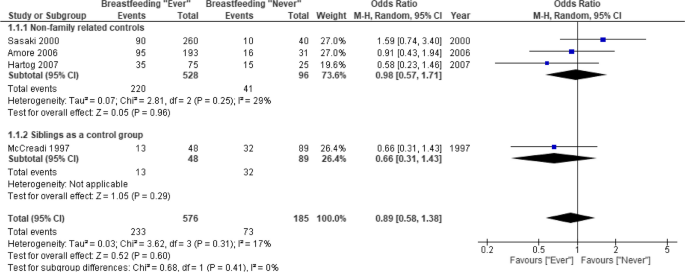
Heterogeneity in methodology and lack of relevant outcome reporting did not allow for meta-analysis of the data from cohort studies. The pooled data from three case–control studies (n = 528) showed no significant association between breastfeeding and schizophrenia later in life OR 0.98 (95% CI 0.57–1.71) [28,29,30] (Fig. 2). In the sensitivity analysis, addition of another study [37] which used siblings as a control group did not change the results OR 0.89 (95% CI 0.58–1.38). The GRADE certainty of evidence was very low due to risk of bias and serious imprecision (Table 2).
Meta-analysis of case–control studies. Breastfeeding (ever vs. never) and risk of schizophrenia. 1.1.1. Primary analysis, which includes studies using non-family related subjects as a control group. 1.1.2. Sensitivity analysis, which included McCreadi et al. study, which used siblings as a control group
Depressive disorders
Five studies (three retrospective [33, 34, 36], two prospective cohorts [31, 36] and one cross-sectional study with retrospective assessment of the exposure which derived data from the UK biobank cohort [47]) investigated depressive disorders (Table 3).
A wide range of instruments was used across the studies for outcome assessment: Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) 5.0 [33, 45], Child Behaviour Check List (CBCL) which is very consistent with DSM-V diagnostic categories [34]. Other scales included PHQ-9 (self-reported Patient Health Questionnaire-9) that is consistent with DSM-IV [40, 47] and Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) which is compatible with DSM-III [36]. According to PHQ-9, depression was defined as having a total score of 11 or more mapping on to DSM-IV [40]. De Mola et al. used Beck’s Depression Inventory (BDI-II) validated for Brazilian population to assess severity of depressive symptoms [45].
The study risk of bias was satisfactory on average, ranging between 4 and 7 as per NOS.
Kwok et al. and De Mola et al. reported no association between breastfeeding and depressive disorders development [40, 45] upon adjustment for multiple potential confounders. Other two studies showed that absence of any breastfeeding was associated with an increased risk (adjOR 1.88 (95% CI 1.28–2.49 and adjOR 1.71 (95% CI 1.14–2.56) respectively) of depressive disorders later on in life (6–16 years of age) [33, 36]. Huang et al. reported a protective effect of breastfeeding only in children who were breastfed longer than 6 months compared to those who have never been breastfed adjOR 0.45 (95% CI 0.23–0.91), while shorter duration of breastfeeding was not associated with any protective effect adjOR 0.79 (95% CI 0.37–1.67) [34]. A very recent cross-sectional study from Liu et al., based on the data from the UK Biobank cohort suggested protective effect of breastfeeding in mothers smoking adjOR 0.86 (95% CI 0.82–0.91) and not smoking adjOR 0.82 (95% CI 0.79–0.84) during pregnancy [47]. The overall GRADE certainty of evidence was very low due to potential risk of bias, serious inconsistency and indirectness (Table 2).
There was a lack of studies reporting the number of participants in the exposed and non-exposed groups to conduct meta-analysis.
Anxiety disorders
Three studies (one case–control [31], one prospective cohort study [36] and one cross-sectional study with retrospective assessment of the exposure using the data from the UK biobank cohort [47]) investigated association between breastfeeding and anxiety disorders [22, 36] (Table 4).
For the primary outcome assessment, Orengul et al. investigated social anxiety disorder, unspecified anxiety disorders, generalised anxiety disorder, specific phobias, separation anxiety disorder and panic disorder using Schedule for affective disorders and schizophrenia for school-age children, present version (K-SADS-P), and the Revised Child Anxiety and Depression Scale (RCADS), total anxiety subscale [31], while De Mola et al. studied generalised anxiety disorder and social anxiety disorder using Mini International Neuropsychiatric Interview version 5.0 validated for Brazil [45].
The risk of bias of the studies varied from unsatisfactory to good.
De Mola and co-authors in their cohort study found no association between breastfeeding or its’ duration and anxiety disorders development [45], while a case–control study from Orengul et al. [31] found reduced risk in breastfed children when compared with those who have never been exposed to breast milk OR 0.17 (95% CI 0.05–0.60). Liu et al. found that breastfeeding in mothers smoking adjOR 0.87 (95% CI 0.79–0.87) and not smoking adjOR 0.83 (95% CI 0.79–0.87) during pregnancy being associated with less anxiety in a cross-sectional study based on the data from the UK Biobank cohort [47]. The overall GRADE certainty of evidence was very low due to potential risk of bias and serious inconsistency (Table 2).
There was a lack of studies reporting the number of participants in the exposed and non-exposed groups to conduct meta-analysis.
Depressive/anxiety disorders as a composite outcome
Two cohort studies assessed anxiety and depression as a composite outcome. Hayatbakhsh and co-authors used the Youth Self Report (YSR) of the Child Behaviour Check List (CBCL) which has the same format as the CBCL but with questions paraphrased in the first person [41]. Oddy et al. reported composite outcome “internalising complaints” that included withdrawn, somatic complaints, anxiety, and depression [43]. Hayatbakhsh et al. found breastfeeding for at least 4 months to be associated with lower scores of CBCL “anxiety/depression” domain at 14 years of age, while Oddy et al. reported breastfeeding for less than 6 months being associated with higher risk of internalising complaints OR 1.21 (95% CI 1.0–1.46).
There was a lack of studies reporting the number of participants in the exposed and non-exposed groups to conduct meta-analysis.
Other mental health disorders
Other conditions investigated in the reviewed manuscripts included borderline personality disorder (BPD) [27] and eating disorders [42] (Table 5).
In a case–control study, Schwarze et al. investigated BPD defined as a pervasive pattern of impulsivity, emotional instability, identity disturbance and dysfunctional interpersonal relationships and diagnosed according to DSM-IV criteria for BPD [27]. Authors reported increased odds of BPD in those who have never been breastfed adjOR 4.68 (95% CI 1.88–11.66).
In a cohort study, Iron-Segev et al. assessed a broad range of eating disorders, including bulimic behaviours like purging, binge eating and other self-reported eating disorders like anorexia nervosa and bulimia nervosa. Purging was defined as using laxatives or force vomiting to lose weight or keep from gaining weight more than one time a month. The patient was considered as binge eater if eating binge at least once a month and feeling out of control while doing so was reported [42]. The study did not find any associations between breastfeeding duration (< 4 months, 4–9 months, > 9 months) and any eating disorder.
There was a lack of studies reporting the number of participants in the exposed and non-exposed groups to conduct meta-analysis.
Association between breastfeeding and maternal mental health
Three studies (a retrospective [35] and two prospective cohorts [39, 46]) investigated associations between breastfeeding and long-term development of maternal mental health outcomes post lactation (Table 6). Among them, one looked at a variety of mental disorders, including schizophrenia, unipolar depression, bipolar affective disorder and anxiety disorders [46] and two assessed associations with maternal depression [35, 39].
For depression assessment, instruments used included Patient Health Questionnaire 9 (PHQ-9), with scores of 10 or higher indicating depression [35], Edinburgh Postnatal Depression Scale (EPDS), with a cut-off of 10 scores being considered a minor depression [39] and ICD-10 codes at admission for each diagnosis of interest [46].
The study risk of bias determined by means of NOS varied from satisfactory to good.
Xu et. al reported association between absence of breastfeeding at the time of hospital discharge and higher risk of schizophrenia adjOR 2.0 (95% CI 1.3–3.1) and bipolar affective disorder adjOR 1.9 (95% CI 1.1–3.5) 12 months after delivery but found no protective effect against anxiety disorders and unipolar depression [46].
Park et al. reported protective effect of prolonged (> 47 months) breastfeeding against maternal depression in the postmenopausal period adjOR 0.33 (95% CI 0.16–0.68) [35].
Hahn-Holbrook and co-authors suggested that women who breastfed more frequently at 3 months postpartum showed greater subsequent declines in depressive symptomatology over time compared to women who breastfed less frequently and lower absolute levels of depressive symptoms by 24 months since birth [39].
Heterogeneity in outcome assessment did not allow for meta-analysis.
Discussion
Breastfeeding has been shown to have a number of benefits for both mother and child. This systematic review assessed up-to-date evidence regarding breastfeeding association with mental health disorders in mother and child. Overall, the current evidence suggests that there is very weak or no association between breastfeeding and the development of mental health disorders. This conclusion is supported by the findings from several studies, including three studies that reported no association between breastfeeding and schizophrenia development in later life (very low evidence). There is conflicting evidence when it comes to associations between breastfeeding and the development of depressive and anxiety disorders, with some studies showing a small protective effect and others reporting no effect. Published literature on this topic has substantial methodological limitations that make it difficult to draw firm conclusions. As it is very hard to randomise breastfeeding exposure, particularly from the ethical perspective, all available evidence comes from observational research only. The GRADE assessment we provide serves a reflection of this limitation and possible biases.
In the published literature, several studies have examined the potential associations between breastfeeding and mental health disorders in both children and mothers. Among studies looking at outcomes in offspring, the majority assessed depressive disorders, schizophrenia and anxiety disorders. Single studies evaluated eating and borderline personality disorders. A small number of studies evaluated associations between breastfeeding and maternal mental health disorders, such as schizophrenia, bipolar affective disorder, anxiety disorders and depression.
Association between breastfeeding and mental health in children
Schizophrenia was the outcome most often reported, with six studies investigating the potential association between breastfeeding and this disease using a variety of methodologies including case–control and cohort designs. The risk of bias of these studies was generally good for the cohort studies and satisfactory to good for the case–control studies, although several studies did not adequately adjust for potentially significant confounders such as family history of schizophrenia. Exposure to breastfeeding was self-reported by parents in most of these studies, and the recall period in some of the case–control studies exceeded 20 years. Overall, most of the studies found no significant association between breastfeeding and schizophrenia. Our meta-analyses of case–control studies demonstrated null effect. However, it is worth noting that a major limitation of case–control studies was lack of adjustment for confounding factors. Due to a small number of cohort studies reporting breastfeeding and schizophrenia, and heterogeneity in outcome reporting, we were unable to perform a meta-analysis. The only study reporting protective effect of breastfeeding for more than two weeks was the Copenhagen Perinatal Cohort [38].
Five cohort studies have investigated the potential association between breastfeeding and the development of depressive disorders in children. The risk of bias of these studies was satisfactory on average, according to the NOS. Two large cohort studies reported no effect, upon adjustment for multiple potential confounders. Two other studies found that an absence of exposure to breastfeeding was associated with an increased risk of developing depressive disorders later in life [33, 36]. The fifth study reported a protective effect of breastfeeding on the development of depressive disorders, but only in children who were breastfed for longer than 6 months, while shorter duration of breastfeeding was not associated with any protective effect [34]. We noted a substantial heterogeneity in approaches to the data collection, differing confounding factors used for adjustment and the outcome assessment with a variety of instruments used which may partially explain contrasting results. A large cross-sectional study with retrospective assessment of the exposure using the data from the UK biobank cohort found that breastfeeding is associated with a lower risk of depression development later in life. The major limitation of this study was related to collection of the data on breastfeeding with participants been asked of whether they were breastfed in their infancy [47]. Such data, based on individuals’ memories in their adulthood, is associated with a substantial risk of recall bias.
Three studies of varied methodologies and potential bias investigated the relationship between breastfeeding and anxiety disorders. The studies used different assessment tools and focused on various forms of anxiety disorders. De Mola et al. cohort study found no correlation between breastfeeding (or its duration) and the development of anxiety disorders [45]. In contrast, the case–control study by Orengul et al. found a decreased risk of anxiety disorders in children who were breastfed as opposed to those who were not [31]. In another cross-sectional study using data from the UK Biobank cohort, Liu et al. discovered an association between breastfeeding and reduced anxiety, irrespective of whether the mothers smoked during pregnancy or not [47], but study design was prone to substantial risk of bias described in a previous paragraph.
Very limited data are available regarding breastfeeding associations with eating disorders and borderline personality disorders. Iron-Segev and co-authors analysed data from the large prospective cohort study of children who are the offspring of female registered nurses participating in the Nurses’ Health Study II (NHS II) and found no associations between breastfeeding and eating disorders. Participant enrolment in the study at the child’s age of at least 9 years, lack of the data regarding infancy and childhood factors are among the primary limitations of this study. The selected sample represents nurses, predominantly white, from a middle and high socioeconomic status, which limit generalisability of the results. One small case–control study showed association between lack of breastfeeding exposure and development of borderline personality disorder development later in life. Reported confidence intervals were very wide and reflect small sample size which restricts extrapolation of these results to other populations.
Association between breastfeeding and maternal mental health
A recent systematic review found an association between breastfeeding and a reduced risk of postpartum depression [22], but it is unclear if this effect persists beyond the first few months of a child’s life. Our review identified only three studies that examined the long-term effects of breastfeeding on maternal mental health. These studies were all cohort studies and used different methods to assess breastfeeding exposure and examined a range of mental health disorders. One large cohort study from Australia found that never breastfeeding was associated with a higher risk of hospitalisation for schizophrenia, bipolar affective disorders and substance-induced mental illness in the first year postpartum compared to women who breastfed their children [46]. Two other studies focused on breastfeeding duration. A small study from the USA found that women who breastfed more frequently at 3 months postpartum experienced a greater decline in depressive symptoms over time [39]. However, it is unclear if the sample size was sufficient for the analyses used and the study had limitations, including the use of self-report measures and a predominantly white, upper-middle class and married sample. A study in South Korea found that a longer cumulative duration of breastfeeding was associated with a decreased risk of postmenopausal depression [35]. However, this study also had limitations, including self-report measures. There is an apparent lack of understanding about the potential association between breastfeeding and long-term maternal mental health. There is a need for more high-quality research to examine the potential association between breastfeeding and long-term maternal mental health. This research should use rigorous methods to assess breastfeeding exposure and control for potential confounders, as well as examine a range of mental health outcomes. Additionally, research should consider the potential moderating factors that may influence the relationship between breastfeeding and maternal mental health, such as individual characteristics, social support and parenting stress.
The GRADE certainty of evidence for all the studied outcomes was very low. This means that there is a high degree of uncertainty about the results, and more high-quality research is needed to confirm these findings. Primary factors that can contribute to a very low GRADE certainty of evidence include risk of bias, serious imprecision, serious inconsistency and indirectness. The very low GRADE certainty suggests that there is a high degree of uncertainty about the results, and more research is needed to confirm these findings.
Limitations
While the current evidence suggests that there is very weak or no association between breastfeeding and the development of mental health disorders, the review has several limitations that should be considered. First, there is a limited availability of high-quality studies that can provide conclusive evidence of the association between breastfeeding and mental health disorders. The current evidence base is primarily based on observational studies, which are subject to a higher risk of bias and confounding factors than randomised controlled trials. Additionally, there is heterogeneity in the study designs and outcomes, making it difficult to compare results across studies. Second, the studies included in this review may be subject to potential biases and confounding factors, such as recall bias or unmeasured confounding variables that were not accounted for in the studies. The studies may also have limitations in the way they assessed and reported breastfeeding exposure. It is also worth noting that the studies included may not be representative of all populations or settings, as the majority of the studies included predominantly white, middle and high socio-economic status individuals. Third, there is a lack of consistent evidence for some mental health outcomes, such as eating disorders and borderline personality disorder. There is also limited evidence available regarding the long-term effects of breastfeeding on maternal mental health. The GRADE certainty of evidence for all the studied outcomes was very low, indicating a high degree of uncertainty about the results and a need for more high-quality research to confirm these findings. Fourth, potential gaps may be associated with our exclusive focus on Medline and Embase databases, without incorporating insights from other relevant databases such as Scopus, CINHAL and PsycINFO, which might offer a broader perspective from allied health and social sciences. Abovementioned limitations should be carefully considered when interpreting the results presented in this manuscript.
Potential directions for future research
Future work in the field may focus on the standardisation of definitions of breastfeeding and the use of consistent, validated tools for the assessment of mental health outcomes. Ideally, future research should consider prioritising cohort studies with larger sample sizes and longer, more regular, follow-up periods, to better understand the long-term implications of breastfeeding on mental health. As most studies lack comprehensive data pertaining to infant exposure to colostrum, and the definition of breastfeeding is frequently imprecise or unclear, there is an area for improvement. Consideration of potential confounding factors, such as family history of mental health disorders, is also crucial to ensure the validity of the findings, as lack of control for confounders was apparent in some of the published research.
Further research is particularly needed in relation to less frequently investigated mental health disorders, as well as in relation to maternal mental health outcomes. There is also a need for more diverse research populations, as most of existing studies were conducted in European and Australasian regions, potentially limiting the generalisability of the findings. Although very costly, development of international consortia focused on prospective, register-oriented data collection could improve the knowledge in the field. A policy-driven, comprehensive data registry for breastfeeding and associated health outcomes could be instrumental for future research.
Despite limited evidence, potential benefits of breastfeeding on the mental health outcomes of both mother and child are apparent due to other known benefits. More efforts should be made that policies should promote and support breastfeeding practices, incorporating robust postpartum mental health screenings and targeted assistance programs for mothers.
Conclusions
There is a lack of consistent evidence to support a relationship between breastfeeding and mental health outcomes in mothers and children. Some studies have found statistically significant associations between breastfeeding and mental health, while others have found no such associations. The quality and methods of these studies are inconsistent, making it difficult to draw conclusions about the relationship between breastfeeding and mental health. Further research is necessary to fully understand any potential associations and potential underlying mechanisms. While breastfeeding may have various benefits for both mothers and children, more research is needed to determine whether it can protect against the development of mental health disorders in both parties.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, DM, upon reasonable request.
Abbreviations
- AAP:
-
American Academy of Pediatrics
- ADHD:
-
Attention deficit hyperactivity disorders
- adjOR:
-
Adjusted odds ratio
- ASD:
-
Autism spectrum disorders
- BDI:
-
Beck’s Depression Inventory
- BPD:
-
Borderline personality disorder
- CBCL:
-
Child Behaviour Check List
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- ECPH:
-
European Commission for Public Health
- EPDS:
-
Edinburgh Postnatal Depression Scale
- GRADE:
-
Grading of Recommendations, Assessment and Evaluation
- GUTS:
-
Growing Up Today Study
- ICD:
-
International Classification of Diseases
- K-SADS:
-
Schedule for Affective Disorders and Schizophrenia for School-Age Children
- LC-PUFAs:
-
Long-chain polyunsaturated fatty acids
- MeSH:
-
Medical subject headings
- MINI-KID:
-
Mini International Neuropsychiatric Interview for Children and Adolescents
- NOS:
-
Newcastle-Ottawa Scale
- NPQ-PSQ:
-
Pre-/Postnatal Stress Questionnaire
- OR:
-
Odds ratio
- PHQ-9:
-
Patient Health Questionnaire-9
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCADS:
-
Revised Child Anxiety and Depression Scale
- RCT:
-
Randomised controlled trial
- ROBINS:
-
Risk Of Bias In Non-randomised Studies—of Interventions
- UK:
-
United Kingdom
- WHO:
-
World Health Organization
- YSR:
-
Youth Self Report
References
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–41.
Mental GBD, Collaborators D. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50. https://doi.org/10.1016/S2215-0366(21)00395-3.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858.
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Sickel AE, Seacat JD, Nabors NA. Mental health stigma update: a review of consequences. Adv Ment Heal. 2014;12(3):202–15.
Das J, Do QT, Friedman J, McKenzie D, Scott K. Mental health and poverty in developing countries: revisiting the relationship. Soc Sci Med. 2007;65(3):467–80.
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–95.
Moreno JL, Kurita M, Holloway T, López J, Cadagan R, Martínez-Sobrido L, et al. Maternal influenza viral infection causes schizophrenia-like alterations of 5-HT2Aand mGlu2 receptors in the adult offspring. J Neurosci. 2011;31(5):1863–72.
WHO. Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services . World Health OrganizationWHO. 2017. p. 1–136. Available from: https://apps.who.int/iris/bitstream/handle/10665/259386/9789241550086-eng.pdf.
Cattaneo A, Yngve A, Koletzko B, Guzman LR. Protection, promotion and support of breastfeeding in Europe. Public Health Nutr. 2005;8(1):39–46.
Meek JY, Noble L. Policy statement: breastfeeding and the use of human milk. Pediatrics. 2022;150(1):1–15.
Bar S, Milanaik R, Adesman A. Long-term neurodevelopmental benefits of breastfeeding. Curr Opin Pediatr. 2016;4:559.
Turner S, Mayumi Maruyama J, Matijasevich A, Pastor-Valero M. Breastfeeding and the development of socio-emotional competencies: a systematic review. Breastfeed Med. 2019;14(10):691–704.
Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61:977.
Devlin AM, Chau CMY, Dyer R, Matheson J, McCarthy D, Yurko-Mauro K, et al. Developmental outcomes at 24 months of age in toddlers supplemented with arachidonic acid and docosahexaenoic acid: results of a double blind randomized, controlled trial. Nutrients. 2017;9:975.
Lassek WD, Gaulin SJC. Maternal milk DHA content predicts cognitive performance in a sample of 28 nations. Matern Child Nutr. 2015;11:773.
Linde K, Lehnig F, Nagl M, Kersting A. The association between breastfeeding and attachment: a systematic review. Midwifery. 2020;81:102592. https://doi.org/10.1016/j.midw.2019.102592.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Tseng PT, Yen CF, Chen YW, Stubbs B, Carvalho AF, Whiteley P, et al. Maternal breastfeeding and attention-deficit/hyperactivity disorder in children: a meta-analysis. Eur Child Adolesc Psychiatry. 2019;28(1):19–30. https://doi.org/10.1007/s00787-018-1182-4.
Tseng PT, Chen YW, Stubbs B, Carvalho AF, Whiteley P, Tang CH, et al. Maternal breastfeeding and autism spectrum disorder in children: a systematic review and meta-analysis. Nutr Neurosci. 2019;22(5):354–62. https://doi.org/10.1080/1028415X.2017.1388598.
Singh GK, Kenney MK, Ghandour RM, Kogan MD, Lu MC. Mental health outcomes in US children and adolescents born prematurely or with low birthweight. Depress Res Treat. 2013;2013:7–18.
Alimi R, Azmoude E, Moradi M, Zamani M. The association of breastfeeding with a reduced risk of postpartum depression: a systematic review and meta-analysis. Breastfeed Med. 2022;17(4):290–6. https://doi.org/10.1089/bfm.2021.0183.
GA Wells, B Shea, D O’Connell, J Peterson, V Welch, M Losos PT. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Zhang Y, Huang L, Wang D, Ren P, Hong Q, Kang D. The ROBINS-I and the NOS had similar reliability but differed in applicability: a random sampling observational studies of systematic reviews/meta-analysis. J Evid Based Med. 2021;14(2):112–22.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJGWG. GrADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Morche J, Freitag S, Hoffmann F, Rissling O, Langer G, Nußbaumer-Streit B, et al. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Z Evid Fortbild Qual Gesundhwes. 2020;150–152:124–33.
Schwarze CE, Hellhammer DH, Stroehle V, Lieb K, Mobascher A. Lack of Breastfeeding: A Potential Risk Factor in the Multifactorial Genesis of Borderline Personality Disorder and Impaired Maternal Bonding. J Pers Disord. 2015;29(5):610–26. https://doi.org/10.1521/pedi_2014_28_160.
Hartong M, Oosthuizen P, Emsley R. Longer duration of breastfeeding associated with risk of developing schizophrenia. S Afr J Psychiatry. 2007;13(2):4. https://doi.org/10.4102/sajpsychiatry.v13i2.30.
Sasaki T, Okazaki Y, Akaho R, Masui K, Harada S, Lee I, et al. Type of feeding during infancy and later development of schizophrenia. Schizophr Res. 2000;42(1):79–82. https://doi.org/10.1016/s0920-9964(99)00102-4.
Amore M, Balista C, McCreadie RG, Cimmino C, Pisani F, Bevilacqua G, Ferrari G. Can breast-feeding protect against schizophrenia? Case-control Study. Biol Neonate. 2003;83(2):97–101. https://doi.org/10.1159/000067960.
Orengul AC, Tarakcioglu MC, Gormez V, Akkoyun S, Zorlu A, Aliyeva N, et al. Duration of Breastfeeding, Bottle-Feeding, and Parafunctional Oral Habits in Relation to Anxiety Disorders Among Children. Breastfeed Med. 2019;14(1):57–62. https://doi.org/10.1089/bfm.2018.0013.
Leask SJ, Done DJ, Crow TJ, Richards M, Jones PB. No association between breast-feeding and adult psychosis in two national birth cohorts. Br J Psychiatry. 2000;177:218–21. https://doi.org/10.1192/bjp.177.3.218.
Zhong BL, Ding J, Chen HH, Li Y, Xu HM, Tong J, et al. Depressive disorders among children in the transforming China: an epidemiological survey of prevalence, correlates, and service use. Depress Anxiety. 2013;30(9):881–92. https://doi.org/10.1002/da.22109.
Huang T, Yue Y, Wang H, Zheng J, Chen Z, Chen T, et al. Infant Breastfeeding and Behavioral Disorders in School-Age Children. Breastfeed Med. 2019;14(2):115–20. https://doi.org/10.1089/bfm.2018.0151.
Park S, Choi NK. Breastfeeding reduces risk of depression later in life in the postmenopausal period: A Korean population-based study. J Affect Disord. 2019;248:13–7. https://doi.org/10.1016/j.jad.2018.12.081.
Allen NB, Lewinsohn PM, Seeley JR. Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Dev Psychopathol. 1998;10(3):513–29. https://doi.org/10.1017/s0954579498001722.
McCreadie RG. The Nithsdale Schizophrenia Surveys. 16. Breast-feeding and schizophrenia: preliminary results and hypotheses. Br J Psychiatry. 1997;170:334–7. https://doi.org/10.1192/bjp.170.4.334.
Sørensen HJ, Mortensen EL, Reinisch JM, Mednick SA. Breastfeeding and risk of schizophrenia in the Copenhagen Perinatal Cohort. Acta Psychiatr Scand. 2005;112(1):26–9. https://doi.org/10.1111/j.1600-0447.2005.00548.x.
Hahn-Holbrook J, Haselton MG, Dunkel Schetter C, Glynn LM. Does breastfeeding offer protection against maternal depressive symptomatology?: A prospective study from pregnancy to 2 years after birth. Arch Womens Ment Health. 2013;16(5):411–22. https://doi.org/10.1007/s00737-013-0348-9.
Kwok MK, Leung GM, Schooling CM. Breast feeding and early adolescent behaviour, self-esteem and depression: Hong Kong's 'Children of 1997' birth cohort. Arch Dis Child. 2013;98(11):887–94. https://doi.org/10.1136/archdischild-2013-304250.
Hayatbakhsh MR, O'Callaghan MJ, Bor W, Williams GM, Najman JM. Association of breastfeeding and adolescents' psychopathology: a large prospective study. Breastfeed Med. 2012;7(6):480–6. https://doi.org/10.1089/bfm.2011.0136.
Iron-Segev S, Peterson KE, Gillman MW, Williams CM, Austin SB, Field AE. Associations of breastfeeding with bulimic behaviors and eating disorders among adolescents. Int J Eat Disord. 2013;46(8):834–40. https://doi.org/10.1002/eat.22165.
Oddy WH, Kendall GE, Li J, Jacoby P, Robinson M, de Klerk NH, et al. The long-term effects of breastfeeding on child and adolescent mental health: a pregnancy cohort study followed for 14 years. J Pediatr. 2010;156(4):568–74. https://doi.org/10.1016/j.jpeds.2009.10.020.
Delgado CA, Munhoz TN, Santos IS, Barros FC, Matijasevich A. Prolonged breastfeeding for 24 months or more and mental health at 6 years of age: evidence from the 2004 Pelotas Birth Cohort Study, Brazil. Child Adolesc Ment Health. 2017;22(4):209–15. https://doi.org/10.1111/camh.12224.
Loret de Mola C, Horta BL, Gonçalves H, Quevedo Lde A, Pinheiro R, Gigante DP, et al. Breastfeeding and mental health in adulthood: A birth cohort study in Brazil. J Affect Disord. 2016;202:115–9. https://doi.org/10.1016/j.jad.2016.05.055.
Xu F, Li Z, Binns C, Bonello M, Austin MP, Sullivan E. Does infant feeding method impact on maternal mental health? Breastfeed Med. 2014;9(4):215–21. https://doi.org/10.1089/bfm.2013.0142.
Liu L, Cheng S, Wen Y, Jia Y, Cheng B, Meng P, et al. Maternal smoking around birth may lower the protective effects of breastfeeding on anxiety, depression and neuroticism in adult offspring: a UK biobank study. Eur Arch Psychiatry Clin Neurosci. 2023;273(2):481–92. https://doi.org/10.1007/s00406-022-01477-7.
Acknowledgements
Not applicable.
Funding
This study received no external funding.
Author information
Authors and Affiliations
Contributions
PB, IA and RB contributed to the work equally and should be regarded as co-first authors. DM and RJB contributed to the work equally and should be regarded as co-last authors. PB: data curation, methodology, writing—original draft preparation, writing—reviewing and editing. IA: data curation, methodology, writing—reviewing and editing. RB: data curation, methodology, writing—reviewing and editing. IK: data curation, methodology, writing—reviewing and editing. AP: data curation, writing—reviewing and editing. YET: data curation, writing—reviewing and editing. VC: conceptualisation, writing—reviewing and editing. AA: conceptualisation, writing—reviewing and editing. DKC: methodology, writing—reviewing and editing. JG: methodology, writing—reviewing and editing. GT: methodology, writing—reviewing and editing. TN: methodology, writing—reviewing and editing. DB: data curation, writing—reviewing and editing. AM: data curation, writing—reviewing and editing. AK: writing—reviewing and editing. SG: writing—reviewing and editing. EK: writing—reviewing and editing. MZ: conceptualisation, methodology, writing—reviewing and editing. RA: conceptualisation, writing—reviewing and editing. RJB: methodology, writing—reviewing and editing. AG: conceptualisation, methodology, writing—reviewing and editing. DM: conceptualisation; data curation; formal analysis; methodology; project administration; writing-original draft; writing-review and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required for this study as it is a systematic review of previously published literature.
Consent for publication
Not applicable.
Competing interests
The authors declare no support from any organisation for the submitted work. Outside of the submitted work, JG benefit from unrestricted research grants from Danone Nutricia Research to Leipzig University for research into human milk composition within the Ulm Birth Cohort Studies—this work is not related to the present publication; author RJB declares consultancy payment from Cochrane, Wiley and the British Society for Allergy and Clinical Immunology for editorial work and payment for expert witness work in cases involving food anaphylaxis and a disputed infant formula health claim.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Box S1.
Search strategies. Table S1. Newcastle Ottawa Scale (NOS) scoring for the cohort studies. Table S2. Newcastle Ottawa Scale (NOS) scoring for the case-control studies. Table S3. Newcastle Ottawa Scale (NOS) scoring for cross-sectional studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bugaeva, P., Arkusha, I., Bikaev, R. et al. Association of breastfeeding with mental disorders in mother and child: a systematic review and meta-analysis. BMC Med 21, 393 (2023). https://doi.org/10.1186/s12916-023-03071-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-03071-7